The Soft Lens, 50 Years OnCheck out articles commemorating the soft lens's anniversary:Manufacturing a Brand-New Industry Advances in Optics Drive Soft Lens Success Replaceable Lenses, Irreplaceable Progress |
Today, soft contact lenses represent a massive industry that provides a host of innovative options to meet the needs of millions that are comfortable while also providing excellent visual acuity. The range of corrections available has expanded significantly since the birth of the soft contact lens, and discoveries continue to enhance the available offerings. With both daily disposables and longer-wear options, individuals have the opportunity to select a lens that works best for not only their vision but also their lifestyle.
 |
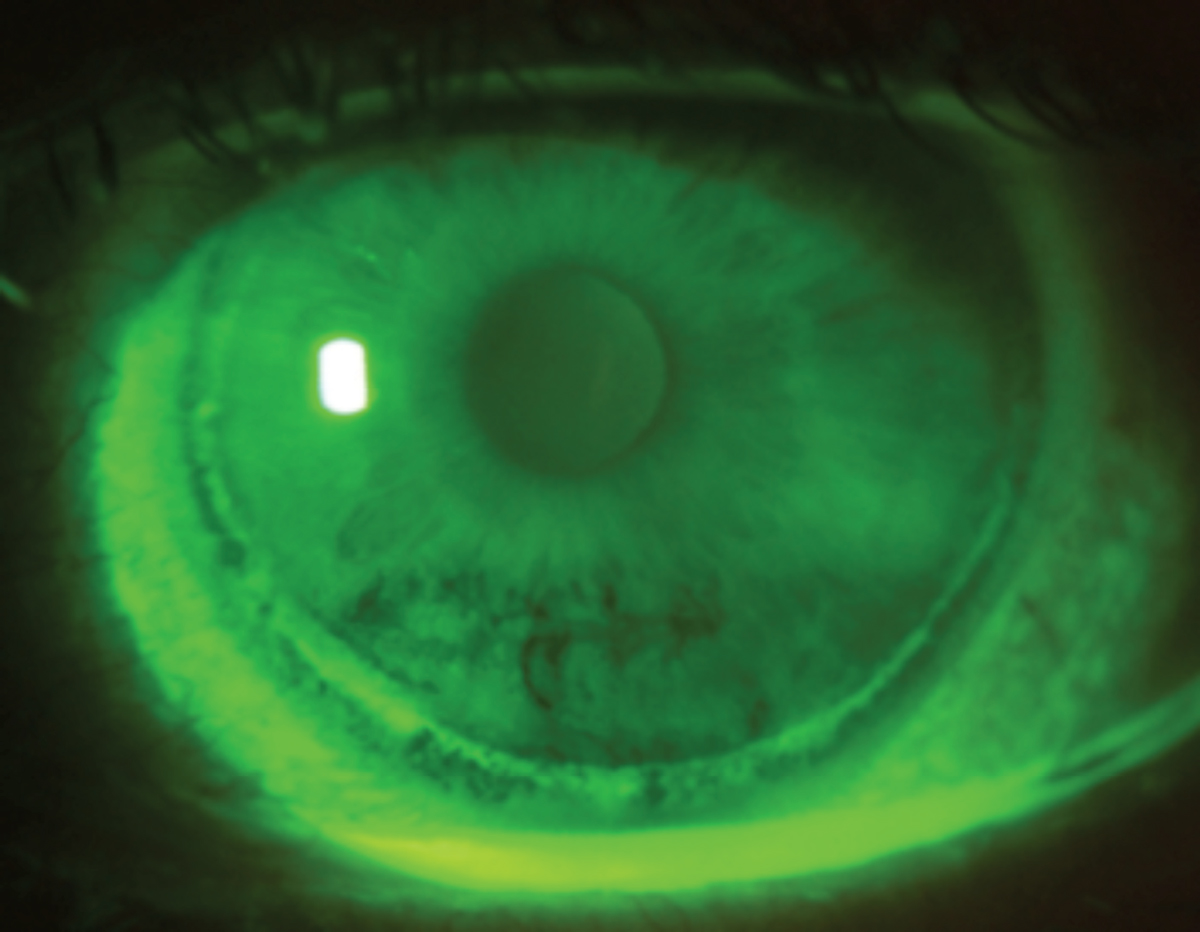
Corneal infiltrate from sleeping overnight in a HEMA material contact lens. Progress in materials science has helped reduce incidence of lens-related complications such as these. Photo: Mile Brujic, OD. Click image to enlarge. |
Since the first soft contact lens was approved by the Food and Drug Administration 50 years ago, the market has grown exponentially, and significant technological advancements have occurred to get us to where we are now. The journey to FDA approval began in the late 1950s/early 1960s with Otto Wichterle, a chemist based in Prague, Czechoslovakia. Professor Wichterle, with his assistant Drahoslav Lim, developed hydroxyethylmethacrylate (HEMA) and recognized this new polymer’s potential as a contact lens material.1
The US government decided in 1968 that soft hydrogel lenses should be classified as a drug and, therefore, would require FDA approval.2 In late 1971, Bausch + Lomb received marketing approval for the Soflens (polymacon). Within one year, three soft lens materials were available in the United States. There were 35 by 1994, and in 2010 the number of soft contact lens materials had reached 90.3
Today we have over 160 different soft contact lens brands in different modalities available in spherical, toric, multifocal and specialty designs. The current lenses meet the many needs of consumers while pushing the boundaries of innovation.
 |
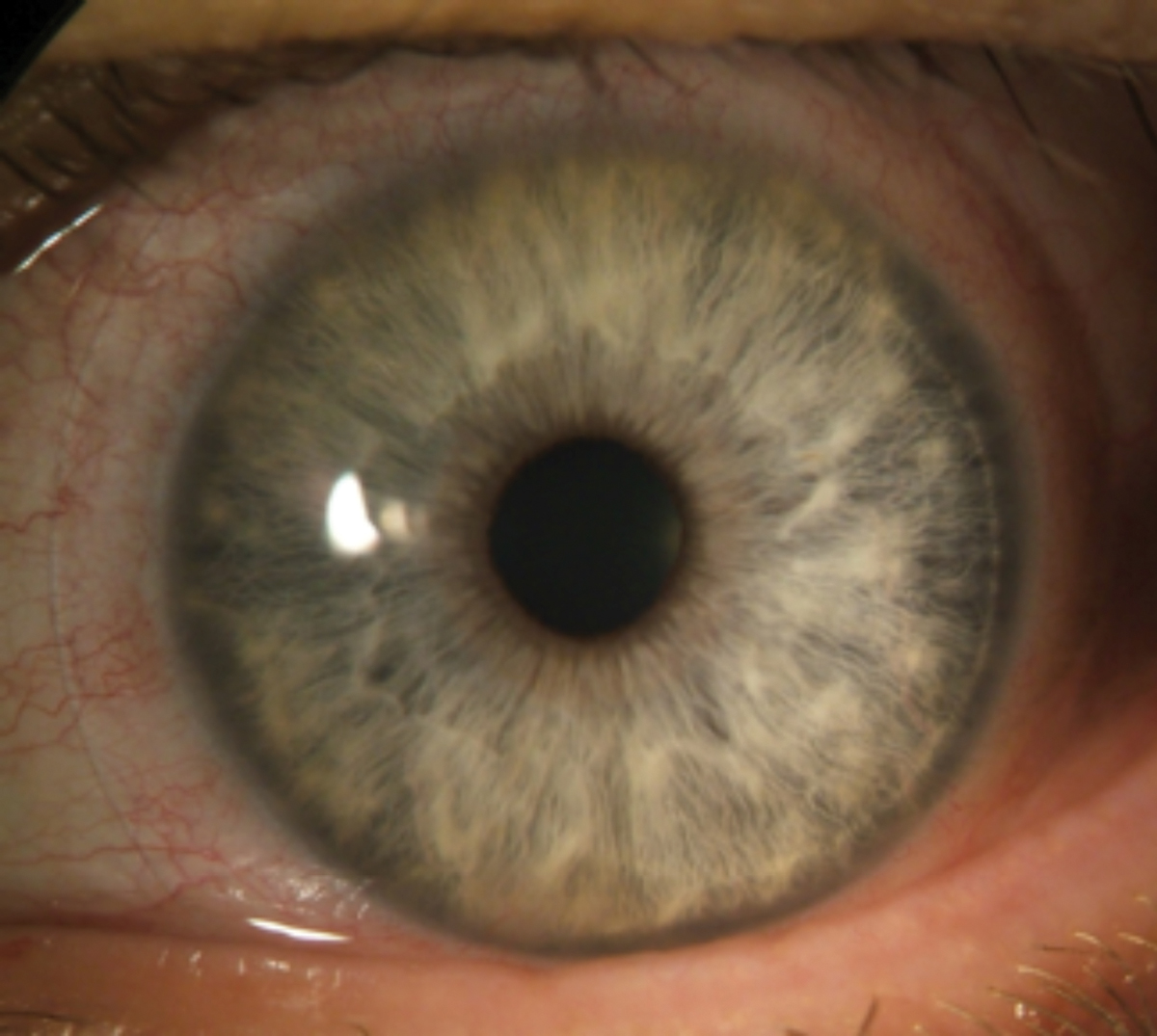
Even though the introduction of silicone hydrogel lenses achieved notable benefits for eye health, the material is still susceptible to complications, especially when worn beyond the recommended wear schedule, and in this case of circumlimbal epithelial splitting from extended wear. Photo: Ken Daniels, OD. Click image to enlarge. |
From Then to Now
The first hydrogel lenses represented a sea change in the contact lens market, offering consumers a level of comfort that had never been available before, compared with their corneal PMMA lenses. This new material revolutionized the field and opened the door to future developments.
“A driving force behind the soft lens was comfort and wearing time,” notes Dwight Akerman, OD, former vice president and global head of professional affairs and business development for Alcon. “Consumers and doctors were amazed at how comfortable soft contact lenses were compared with rigid lenses.”
 |
Contact lens–induced acute red eye response (CLARE) from extended wear SiHy lenses. Photo: Ken Daniels, OD. Click image to enlarge. |
Initially, it was marketed as a yearly replacement lens, Dr. Akerman recalls. And so, wearers had to go through aggressive cleaning regimens to ensure disinfection and to maintain comfort. Patients had to use a contact lens cleaner, then rinse it off with saline before placing it into a heating unit to disinfect the lens. Then, once a week, they would clean the lenses with enzyme tablets to remove protein deposits, according to Karen Yeung, OD, senior optometrist at UCLA’s Arthur Ashe Student Health and Wellness Center. Dr. Yeung notes that homemade saline with salt tablets and distilled water resulted in a high incidence of corneal infections.
“This was the dominant modality for many years; however, it soon became obvious that there were deficiencies with both the material and frequency of replacement,” Dr. Akerman says. “Specifically, there were issues with buildup, especially tear protein on the surface of the contact lens, which can cause irritation and inflammation on the eye.”
The complications associated with hydrogel lens materials, especially protein deposits, could result in a short wearing life. Research found that proteins could begin early. For high-producing patients, deposits could be detected after one minute of wear and within 30 minutes the lenses could begin to spoil. Patients who wore these lenses also experienced neovascularization and papillary conjunctivitis due to inflammation.2
It was the inventor of the soft contact lens himself, Dr. Wichterle, who would first propose the idea of disposable contact lenses. During a 1980 meeting of the International Society for Contact Lens Research, he said, “Once deposits occur, we could reject the lens and take a new one! I believe we are now very close to the development of technology which will cause a dramatic drop in the selling price of lenses. Once you are able to buy a lens for one dollar or less, lens spoilage won’t play a role. If a lens is spoiled, it will be cheaper to buy a new lens than to buy expensive solutions and waste time with cleaning.”2
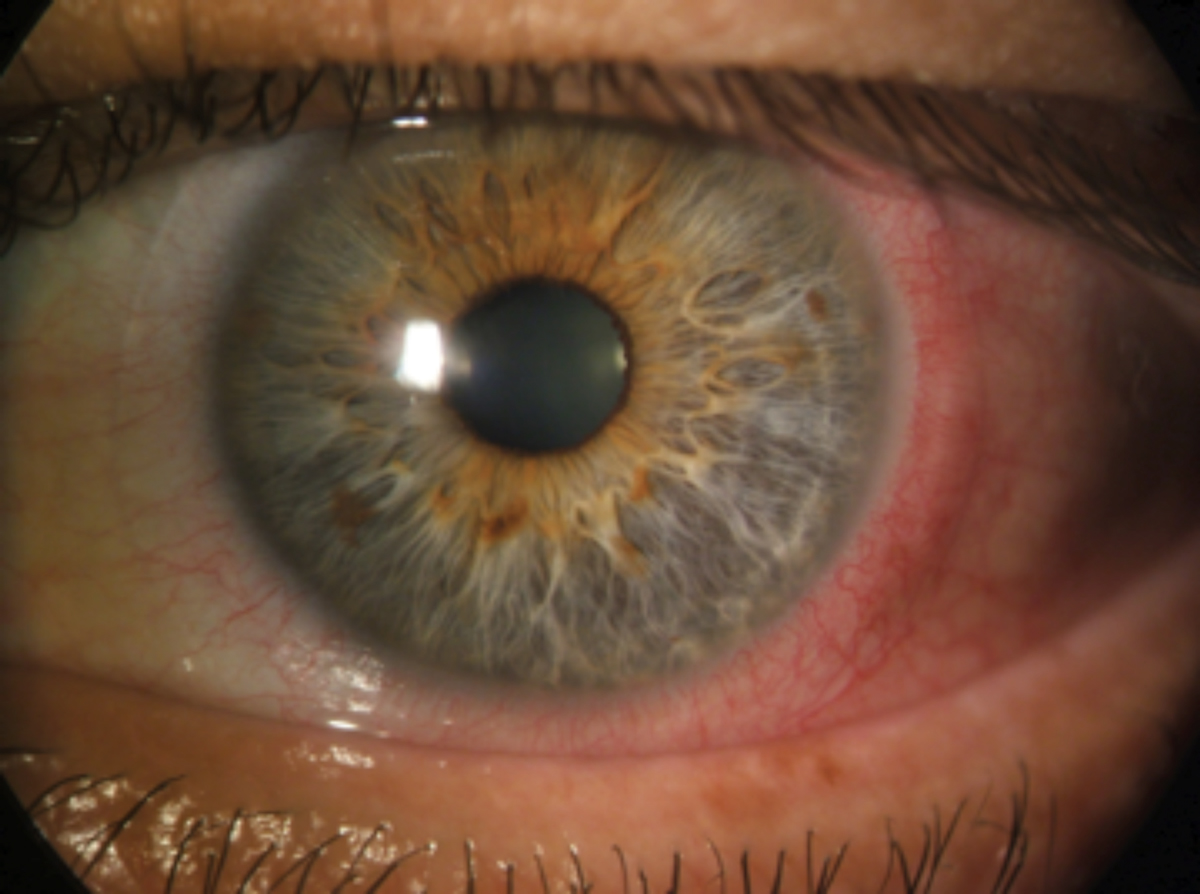 |
CLARE presenting with extreme conjunctival injection in the absence of corneal infiltrates. Photo: Ken Daniels, OD. Click image to enlarge. |
Technology for developing lenses was improving, but it would be many years before his vision became a reality. Soft contact lens manufacturing was still a very manual process in which workers would have to handle every contact lens. In 1987 Vistakon (now Johnson & Johnson Vision Care) was able to mass produce contact lenses more efficiently. Acuvue lenses were first developed as one-week extended wear contact lenses. There was the belief that handling the contact lenses increased the risk of infections, so it would be better to minimize handling by sleeping in the contact lenses and removing the contact lenses in a week. Unfortunately, the rate of infection and complications is much higher with extended wear lenses.
“While some of the HEMA lenses were approved for extended wear, lack of oxygen transmissibility led to irritated eyes and, in some cases, infections,” Dr. Akerman says. “Eyecare professionals actively discouraged patients from wearing these lenses despite FDA approval.”
Extended wear waned in popularity in 1989 when concerns regarding the risk of complications arose. Research showed that the incidence of ulcerative keratitis increased for individuals who wore soft contact lenses for an extended period.4 As a result, manufacturers reduced extended wear from 30 to seven days and included information on risks in their product labeling.3
In 1995, the whole industry changed when Johnson & Johnson introduced the 1-Day Acuvue (etafilcon A) lens, the first daily disposable, notes Lyndon Jones, PhD, FCOptom, director of the Centre for Ocular Research & Education (CORE) at the University of Waterloo.
Research has shown that the prevalence of complications was significantly lower among individuals who wore daily disposable lenses than those who used less disposable and conventional soft daily lenses.5,6 Additionally, researchers have found that patients with disposable daily wear lenses reported symptoms less frequently at routine visits and were less likely to unscheduled visits for complications and symptoms.5
The low oxygen transmissibility of the current soft contact lenses also presented a challenge. Innovations in materials were needed to address this. “While hydrogel lenses offered a new level of comfort, the material suffers from low oxygen transmissibility and deposit buildup, especially tear protein buildup on the surface of the lens,” explains Dr. Akerman. “Therefore, polymer chemists at the various contact lens companies continued to explore ways to address these issues, but it would be quite some time before we saw another major breakthrough in materials.”
The next significant milestone in soft contact lens materials occurred in the late 1990s with the advent of silicone hydrogels. This material sought to bring together the benefits of highly oxygen permeable silicone monomers with the wettability and comfort of hydrogels.
“Silicone hydrogels were an exciting development for eyecare professionals as well as consumers,” Dr. Akerman recalls. “These lenses allowed plenty of oxygen to reach the cornea resulting in white, healthy-looking eyes. This was especially valuable to patients who wore their lenses all day, every day.”
Silicone hydrogels renewed interest in extended wear and, in 2001, the FDA approved the Ciba Vision Night & Day contact lens for up to 30 nights of continuous wear. Approval followed soon after for Bausch + Lomb’s PureVision lens.7 These first-generation silicone contact lenses had a highly rigid modulus due to the high silicone content and low water content, notes Dr. Yeung. “Later generations of silicone contact lenses were more comfortable as the modulus was decreased by lowering the silicone while increasing water content without compromising too much on oxygen transmissibility.”
Selected Highlights in Soft Contact Lens Development1971: FDA approves first soft contact lens (soflens, Bausch + Lomb) 1983: First soft color contact lenses 1987: First disposable soft contact lenses launched 1996: First daily soft disposable contacts were released 1997: First monthly silicone hydrogel contact lenses (Night & Day, Ciba Vision) 2004: Second-generation silicone hydrogel contact lenses (Acuvue Oasys, Johnson & Johnson) 2005: Third-generation silicone hydrogel contact lenses (Biofinity, CooperVision) 2008: Silicone hydrogel daily disposable contact lenses enter the market 2013: First water-gradient soft contact lens material (Dailies Total1, Alcon) 2019: First soft lens approved to slow the progression of myopia in children (MiSight, CooperVision) |
The first daily disposable silicone hydrogel lens was introduced in 2008.8 The convergence of these two paths of innovation—daily disposable replacement and new silicone hydrogel materials—was a turning point for the industry, notes Karen Walsh, MCOptom, a clinical scientist at CORE. With fewer complications compared with reusable lenses, evidence supports the use of daily disposables for many patients. The addition of silicone hydrogel materials offers long-term advantages for a patient’s health.8
“Daily disposable silicone hydrogels were something practitioners had been wanting for years because we could see the advantages they would bring,” Dr. Walsh says. “Since they were introduced, we have witnessed a significant increase over time of available materials and lens designs in this category that can meet the needs of a wide range of patients.”
Today, daily disposable silicone hydrogel lenses are the fastest-growing category in contact lenses worldwide, according to Dr. Akerman, who notes that while an important addition to the market there is still a place for older materials. “They’re still very appropriate for many patients, especially in the daily disposable category. Part-time wearers can benefit from these lenses, which also come at a lower cost.”
Opportunities for Growth
While great strides have been made in the last 50 years, there are still opportunities for growth and improvement in the soft contact lens.
Multifocal and toric soft contact lenses have seen advancements since they were introduced decades ago. In 2002, the first daily disposable astigmatism lens design (Focus Dailies, Ciba Vision) was introduced in 2002. The Focus Dailies Progressives (Ciba Vision) was the first daily multifocal lens. The first disposable presbyopic lens (Acuvue Bifocal, Johnson & Johnson)—a one-week extended wear lens—entered the market in 1998. Focus by Ciba Vision was launched in 1999—the first disposable toric lens with monthly replacement.2
The market continues to expand for these more specialized lenses; however, gaps remain. “Right now, we are only able to correct certain higher order aberrations,” notes Joseph Shovlin, OD, of Scranton, PA, past president of the American Academy of Optometry. “And I think that’s the next frontier: to be able to correct greater aberrations effectively for better acuity—super acuity, if you will.”
There is room to improve the optics of these lenses, Dr. Shovlin suggests, noting that while significant progress has been made correcting astigmatism and there are good options available today, advances are still needed in presbyopic designs. “I believe that is the desire for the future: to find the lens that works for every presbyopic patient,” he says.
This is a challenging endeavor, Dr. Shovlin acknowledges. “The problem with soft lenses is figuring out how to impose the optics to simultaneously correct distance and near vision,” he explains, while also urging practitioners to remember all of the progress that has been made.
“Early on we didn’t even think about correcting astigmatism,” Dr. Shovlin emphasizes. “We didn’t even think about correcting presbyopia. We were just hoping to correct low to moderate amounts of myopia and now we can correct virtually any amount of myopia.”
With today’s lens options, “we can correct high amounts of astigmatism at an around-the-clock axis, and we can find a successful option for patients who are presbyopic, probably about 70% of the time,” he continues. “We’ve got a long way to go, but we’ve come a long way, and I think it’s important to recognize the significant advances that gotten us to where we are today.”
Myopia control with soft contact lenses is another hot topic, notes Dr. Yeung. “Currently the only FDA-approved myopia control contact lens, MiSight by CooperVision, is a one-day HEMA hydrogel contact lens,” she says. “Because the pediatric patients will be wearing contact lenses for many decades, inevitably a one-day disposable silicone myopia control contact lens will emerge in the market.”
Table. Pros & Cons of Soft Lens Materials14 | ||
| Pros | Cons | |
Hydrogels |
|
|
Silicone Hydrogels |
|
|
Ongoing Innovation
Materials scientists continue to look for new ways to both enhance and revolutionize soft contact lenses. There are a number of avenues being explored; some are showing promise now while others may take longer to become a reality.
While silicone hydrogel materials, both in daily disposable and other replacement modalities, have addressed the oxygen transmissibility issues of the early lenses, one area of ongoing focus is comfort.
“Now, the innovations we see from major manufacturers are focused on initial and end-of-day comfort,” notes Dr. Akerman. “Many consumers—especially those who spend most of their time in front of a digital device —still have dryness and discomfort issues, particularly after hours of wear.”
The goal of manufacturers is to make lenses as comfortable at the end of the day as they are when a consumer first puts them in their eye, explains Dr. Akerman, noting a number of recent innovations.
For example, Bausch + Lomb recently introduced the Infuse daily disposable lens, which is designed to address end-of-day discomfort.9 The Precision1 (Alcon) daily disposable lenses were released in the last year. This lens uses a permanent, micro-thin layer of moisture at the lens surface to support a stable tear film.10 Dailies Total1 has a water gradient to improve ocular dryness. Other products designed to improve comfort include the MyDay (CooperVision) and Acuvue Oasys 1-Day (Johnson & Johnson).
“Comfort is king,” emphasizes Dr. Akerman. “And if a patient can’t wear the lenses comfortably all day, they tend to be dissatisfied and frequently will dropout. These innovations also offer improvements to visual acuity, but the number one innovation addresses dryness and comfort.”
Other areas of exploration center on contact lenses as drug delivery systems. Unlike administering agents with eye drops, a drug-loaded contact lens could provide higher drug bioavailability.11 A number of different systems have been explored. For example, a new device has been developed using vitamin E nano-barriers to extend drug release.12
“We are in an exciting era of new technology,” notes Dr. Yeung. “Johnson & Johnson is soon to launch their latest contact lenses pre-loaded with ketotifen, an antihistamine to help contact lens wearers with their ocular allergies. Researchers in the University of Manchester are creating contact lenses to treat corneal melting.
Contact Lenses and the Ocular SurfaceWhile innovations continue to improve the optics and comfort of soft contact lenses, it is important not to forget about the ocular surface. Just as there have been advancements in contact lens materials, significant work has been devoted to helping practitioners improve the ocular surface and tear film. “Despite significant improvements, we still have some comfort issues for patients, especially towards the end of the day,” says Dr. Walsh, who notes that when a patient complains of discomfort, clinicians will often change the lens type and may add a lubricating drop. “We can now be more scientific and much like we would with a dry eye problem, we can address ocular surface-related issues to improve contact lens comfort,” she continues. “As a profession, we are getting better at looking at the whole system when it comes to our patients.” Dr. Jones agreed, while highlighting that dropout rates remain higher than practitioners would like. “We’re still seeing about 20% of patients dropping out and some of that is related to handling issues; however, many are a result of vision and comfort challenges. “You can take the best lens and solution in the world and if you put it into an eye that simply doesn’t have a good ocular surface or a good tear film, it’s probably not going to be successful,” he emphasizes. “This is where optometrists play a key role in helping patients have optimal outcomes.” |
“A new company called Mojo Vision is coming out with smart contact lenses that have a pinpoint computer screen embedded into the contact lenses,” she continues. “The contact lens could have a speech app that allows you to see your pre-written script as you recite it in front of your audience. The Apioc (Lentechs) lens is now undergoing clinical trials for a novel approach to correct for presbyopia with translating soft contact lenses. The list goes on.”
What could the long-term future of soft contact lenses look like? There are a number of possibilities, according to Dr. Yeung. “I can imagine a world where contact lenses just self-disintegrate in the eyes towards the end of the day so that we would never have to deal with patient noncompliance or with plastic waste,” she muses. “Or just a pair of contact lenses that you never have to remove and adapts to our changing prescriptions.
“We, of course, have lots of room for more improvement for the current contact lenses, but we have come a long way and I am looking forward to where things will be in the future.”
Proactive Approach
As advancements continue, the growth of contact lens market depends not only on innovation and new developments but also on the optometrist. The tremendous advances that have occurred since the soft contact lens was first introduced only make a difference if practitioners fit patients, notes Dr. Jones, who encourages ODs to adopt a proactive approach as opposed to waiting for patients to ask for lenses, which will help enhance their practice.
The SynergEyes VS scleral lens was selected for this fitting because it offered desirable qualities and customizable parameters for this patient’s unique corneal condition and aphakic status.
1. McMahon T, Zadnik K. Twenty-five years of contact lenses. Cornea. 2000;19(5):730-40. 2. Parker C, Tison K, Meyers R. Toward disposability of contact lenses. The Contact Lens Museum. To be published. 3. Szczotka-Flynn L, Ahearn D, Barr J. History, evolution, and evolving standards of contact lens care. Cont Lens Anterior Eye. 2013;36(S1):S4-8. 4. Poggio EC, Glynn RJ, Schein OD, et al. The incidence of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. N Engl J Med. 1989;321(12):779-83. 5. Poggio EC, Abelson MB. Complications and symptoms with disposable daily wear contact lenses and conventional soft daily wear contact lenses. CLAO J. 1993;19(2):95-102. 6. Forister JF, Forister EF, Yeung KK, et al. Prevalence of contact lens-related complications: UCLA contact lens study. Eye Contact Lens. 2009;35(4):176-80. 7. Dan DeAngelis D, Carter S. FDA gives CIBA vision preliminary OK for extended wear. Rev Optom. July 24, 2001. www.reviewofoptometry.com/article/fda-gives-ciba-vision-preliminary-ok-for-extended-wear. Accessed March 31, 2021. 8. Sulley A, Dumbleton K. Silicone hydrogel daily disposable benefits: The evidence. Cont Lens Anterior Eye. 2020;43(3):298-307. 9. Bausch + Lomb. Infuse. www.bauschinfuse.com/ecp/. Accessed March 31, 2021. 10. Alcon. Alcon to launch PRECISION1 daily disposable contact lenses as it continues to deliver on vision care pipeline. www.alcon.com/media-release/alcon-launch-precision1-daily-disposable-contact-lenses-it-continues-deliver-vision. Accessed March 31, 2021. 11. Peral A, Martinez-Aguila A, Pastrana C. Contact lenses as drug delivery system for glaucoma: a review. Appl Sci. 2020;10(15):5151. 12. Contact lens drug delivery for glaucoma: A better way to get there. Ophthalmology Times. February 7, 2020. www.ophthalmologytimes.com/view/contact-lens-drug-delivery-glaucoma-better-way-get-there. Accessed March 31, 2021. 13. US Food and Drug Administration. FDA approves first contact lens indicated to slow the progression of nearsightedness in children. November 15, 2019. www.fda.gov/news-events/press-announcements/fda-approves-first-contact-lens-indicated-slow-progression-nearsightedness-children. Accessed March 31, 2021. 14. Musgrave CSA, Fang F. Contact lens materials: a materials science perspective. Materials (Basel). 2019;12(2):261. |


