Each year, the Association for Research in Vision and Ophthalmology (ARVO) annual meeting gifts the eyecare profession with a cornucopia of new research that lets us see where the winds are blowing clinically. Here, we’ve compiled research specific to cornea and contact lens care we feel may be most impactful for practicing optometrists.
This year’s meeting was held in New Orleans from April 23-27. The theme of ARVO 2023 was “the beauty of diversity in science and nature.” The findings summarized here are only a snippet of those presented at the meeting, of course, but show the rich expanse of insights ARVO generates each year.
Cornea
This year’s presenters highlighted a host of new and exciting research from the last 12 months focused on this part of the eye.
Latest ARMOR study updates show multidrug resistance remains common. Treating ocular infections is hard enough as is when the drugs work as advertised, and so much the worse when the offending microorganism is resistant or only weakly susceptible to therapy. Staphylococci are known causative pathogens in ophthalmic infections, and antibiotic resistance among these bacteria is of clinical concern. The long-running Antibiotic Resistance Monitoring in Ocular micRoorganisms (ARMOR) Study, the only nationwide surveillance study of its kind, captures in vitro data specific to common ocular pathogens. The team’s two research posters noted that, with preliminary data indicating lower resistance rates especially among Staphylococcus aureus, multidrug resistance was common among methicillin-resistant strains.
One analysis reported on 2022’s data, when 397 isolates were collected January through October of that year.1 Staphylococcus aureus, coagulase-negative staphylococci (CoNS), Streptococcus pneumoniae, Pseudomonas aeruginosa and Haemophilus influenzae from ocular infections were collected as part of ARMOR and submitted to a central laboratory for species confirmation and in vitro antibiotic susceptibility testing. Minimum inhibitory concentrations for up to 16 antibiotics (10 drug classes) were determined and interpreted.
 |
|
Staphylococcal infections demonstrated greater susceptibility to even some older medications in the newest ARMOR study. Photo: Aaron Bronner, OD. Click image to enlarge. |
The 142 CoNS isolates exhibited the highest resistance, with azithromycin, oxacillin/methicillin, trimethoprim, clindamycin and tetracycline resistance observed in 60%, 37%, 28%, 27% and 22% of isolates, respectively. Among the 161 S. aureus isolates, 46% were resistant to azithromycin, but <20% of isolates were resistant to other drugs. Multidrug resistance (poor or ineffective response to three or more drug classes) was observed in 14% of S. aureus, 39% of CoNS and in 59% and 88% of methicillin-resistant strains thereof, respectively.
Among the five S. pneumoniae isolates, 60% were resistant to azithromycin, oral penicillin and tetracycline. Although all 72 P. aeruginosa isolates were resistant to polymyxin B, <5% were resistant to other drugs; no resistance was found among the 17 H. influenzae isolates.1
“The clinical significance of these in vitro data is unclear without consideration of the ocular pharmacokinetics of tested antibiotics,” the researchers concluded in their abstract.1
The team’s other study examined resistance trends over time among staphylococcal isolates collected from 2009 through 2022 in ARMOR. A total of 2,999 S. aureus and 2,575 CoNS were included in their analysis.2
In vitro resistance decreased to methicillin/oxacillin (S. aureus, 39% in 2009 to 18% in 2022; CoNS, 50% in 2009 to 37% in 2022) and to ciprofloxacin (S. aureus, 39% in 2009 to 17% in 2022; CoNS, 46% in 2009 to 20% in 2022). Also, among S. aureus, resistance to azithromycin decreased (62% in 2009 to 46% and 9% in 2022), as did resistance to tobramycin (24% in 2009 to 9% in 2022); in contrast, an increase in chloramphenicol resistance was observed (7% in 2009 to 3% in 2022, peaking at 30% in 2021). Cumulative multidrug resistance (three or more antibiotic classes) was observed in 30% of S. aureus and 41% of CoNS and in 76% and 79% of methicillin-resistant isolates thereof, respectively.
The researchers also noted that resistance data should be considered in combination with known ocular pharmacokinetics of antibiotics. However, this time they emphasized that practitioners should also consider resistance data when selecting empirical treatment for staphylococcal eye infections in particular.2
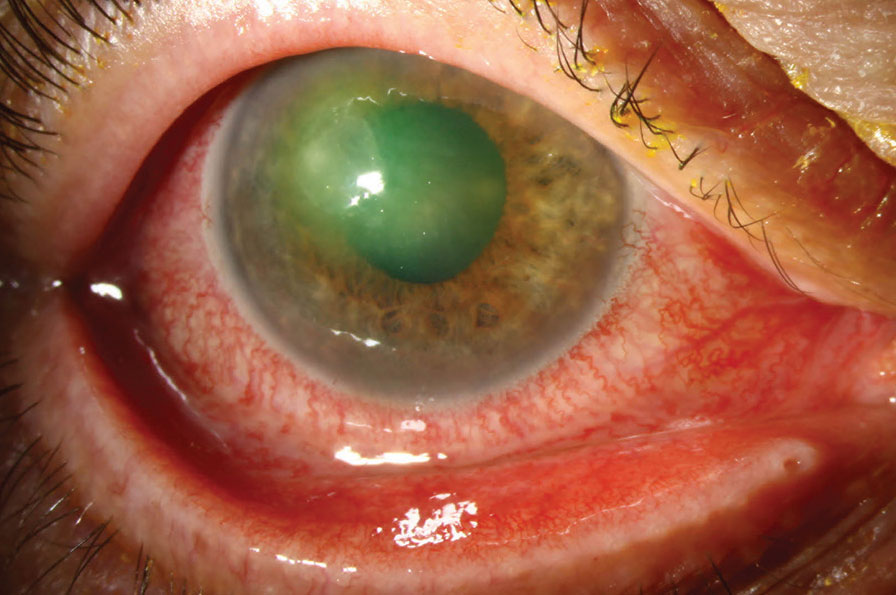
Age, smoking history, Pseudomonas among risk factors infectious keratitis treatment failure. In a retrospective study conducted at the University of Rochester, researchers examined patient demographics, systemic and ocular comorbidities and microbial data to determine which factors, if any, are associated with infectious keratitis.3
The study included 407 patients with infectious keratitis who had clinical follow-up documentation of at least two weeks after diagnosis. Treatment failure was defined as having no clinical improvement within two weeks of initial presentation and/or needing surgical intervention of corneal gluing, patch grafts, transplants or evisceration of the eye.
A small proportion (15.2%) of the 407 participants experienced treatment failure. However, of this group, 58.1% needed surgical intervention. After looking at the different data, researchers found higher rates of Pseudomonas aeruginosa, fungi and polymicrobial cultures. Other risk factors associated with treatment failure were age greater than 65, systemic immunosuppression and history of smoking.
Ocular history associated with treatment failure included previous corneal transplant, previous transplant rejection, topical steroid use, intraocular surgery history and a visual acuity of 20/250 or worse. Higher rates of prescribed fortified antibiotics were given, and more bandage contact lenses were used in patients with treatment failure during treatment.
 |
|
Patients with treatment failure were more prone to have polymicrobial, P. aeruginosa (shown here) or fungal infections. Photo: Christine Sindt, OD. Click image to enlarge. |
As such, the authors noted that many different ocular and other factors put patients at risk of treatment rejection for infectious keratitis. They believe that “this study improves our understanding of infectious keratitis by identifying key prognostic indicators of treatment failure for this blinding disease,” according to their ARVO abstract.
Fuchs’ questionnaire identifies modifiable lifestyle risk factors. Though it’s primarily a genetic condition, Fuchs’ corneal endothelial dystrophy shows some response to several lifestyle factors may also play a role in the disease onset, according to one study. Identifying potentially modifiable risk factors for severe Fuchs’—which requires corneal transplantation—may inform patient counseling for those most at risk.4
The researchers developed a Fuchs’ dystrophy questionnaire (link available online) to assess disease-specific medical history and lifestyle risk factors such as obesity, alcohol use, smoking and sun exposure. The questionnaire was administered to a prospective cohort of patients with Fuchs’ dystrophy who also had an indication for endothelial keratoplasty. These patients underwent slit lamp biomicroscopy with modified Krachmer grading to determine guttae confluence and visible corneal edema.
The questionnaire had an 82% response rate from 375 total participants. The mean age at endothelial keratoplasty was 68 years for both sexes.
No differences in corneal edema incidence were found between smokers and non-smokers or between those with frequent alcohol intake (≥two days/week) and non-frequent drinkers. Interestingly, men were 1.42-times more likely to have corneal edema before endothelial keratoplasty than women, even though more females undergo keratoplasty.
Skin type may also be an indicator of risk. Participants who reported taking strict sun protection measures within minutes of exposure were 1.44-times more likely to have corneal edema than those with an hour or more of unprotected sun exposure. “A possible explanation of increased risk of corneal edema in participants with strict sun protection compared with those without might be that photosensitive skin types are more relevant than direct sun exposure,” the researchers wrote in their abstract.
Finally, for every five-unit increase in BMI, corneal edema was 1.26-times more likely at endothelial keratoplasty but not for a higher BMI at age 21. The researchers wrote that “interventions to reduce obesity in adulthood may modify the risk of Fuchs’ dystrophy severity independent of age, sex and weight in adolescence.”
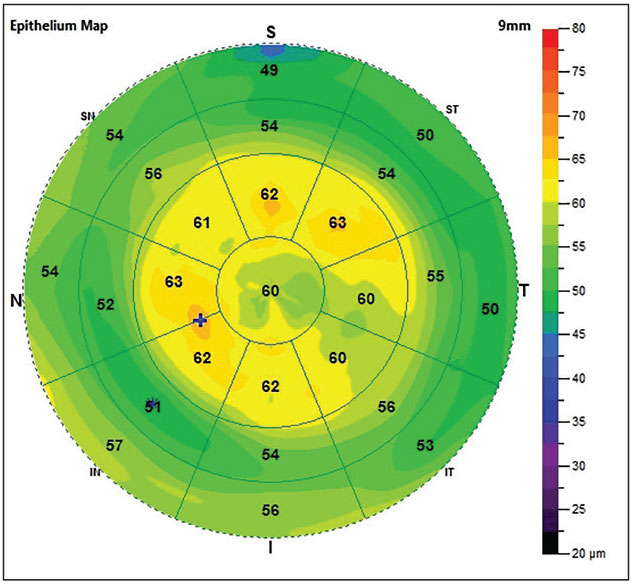
Autoimmune disease associated with superior epithelial thinning. Previous studies have shown that patients with dry eye disease (DED) display thinner superior corneal epithelium compared with normal controls. Researchers recently tested their hypothesis that presence of autoantibodies has been associated with superior epithelial thinning.5 They also assessed the link between corneal epithelial thickness and clinical findings and assessed the utility of including corneal epithelial thickness as a diagnostic tool for patients with DED.
This study included 208 patients who visited the DED clinic at University of Illinois Chicago and had bloodwork results in their medical records for autoantibodies associated with DED-related autoimmune diseases. If available, superior corneal epithelial thickness, Schirmer’s 1 test and corneal higher order aberrations (HOAs) were obtained from the patient’s medical records. Superior corneal epithelial thickness was determined with the RTVue XR OCT Avanti (Visionix) system, and corneal HOAs were determined using the iTrace (Tracey Technologies) system. A decision tree was used to determine feature variables and cutoffs necessary to accurately classify antibody positive and negative groups.
 |
|
If a patient’s eye has both superior corneal epithelial thickness <45µm and Schirmer’s test result <10mm, they are five times more likely to have antibody-positive bloodwork and associated visual compromise. Photo: Justin Cole, OD; Jarett Mazzarella, OD. Click image to enlarge. |
The researchers found that patients with antibody-positive bloodwork had a significantly thinner superior corneal epithelial thickness (47.41µm vs 49.73µm) compared with patients with antibody negative blood work (n=181 eyes).
The top two most useful clinical indicators that a patient will have antibody-positive bloodwork are a Schirmer’s <15mm and an epithelial thickness <45µm. Eyes with epithelial thickness <45µm and Schirmer’s <10mm (n=69 eyes) have significantly greater corneal HOAs (1.85 vs. 0.1) compared with eyes with thickness ≥45µm and/or Schirmer’s ≥10mm (n=164 eyes). If a patient’s eye had both superior corneal epithelial thickness <45µm and Schirmer’s test results <10mm, the probability that they have autoantibody-positive bloodwork was 81.2%.
“Presence of autoimmune disease must be considered in patients who have superior epithelial thinning and reduced tear production because these patients are five-times more likely to have antibody-positive bloodwork and associated visual compromise, as demonstrated by high corneal HOAs,” the researchers concluded.
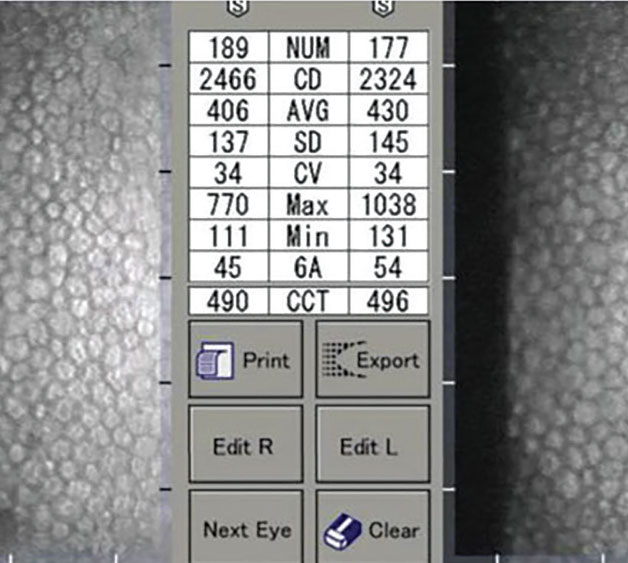
Myopia could affect corneal endothelial morphology. Researchers recently observed greater polymegethism and pleomorphism in healthy eyes with wider mean anterior chamber angle.6 This implies that the corneal endothelial quality tends to be poorer in eyes with wider anterior chamber angle. These eyes are more likely to be myopic, and myopic corneas may be more fragile and more susceptible to mechanical stress.
The study evaluated 272 eyes of 136 Caucasians. Mean age was 46.8, and 61% were men. Significant associations were shown between corneal volume, mean anterior chamber angle, white-to-white distance and age with the morphology of the corneal endothelium. Greater polymegathism was found in older individuals, and greater pleomorphism was found in adults with greater white-to-white distance.
Statistical modeling of the data revealed that mean ECD (2,673.61 cells/mm2) was positively correlated with corneal volume (59.43mm3). After adjusting for age, it was only negatively correlated with age. The coefficient of variation of cell area (28.6%) was positively correlated with mean anterior chamber angle (35.1º). After adjusting for age, the correlation was stronger. Hexagonal cell appearance ratio (67.5%) was negatively correlated with white-to-white distance (11.8mm) and mean anterior chamber angle, and after adjusting for age, this correlation remained the same.
 |
|
Reduced corneal endothelial density could be expected in eyes that develop myopia, one study suggests. Photo: Daniel Epshtein, OD. Click image to enlarge. |
The researchers noted that the exact mechanism by which myopia could cause corneal endothelial morphology change needs to be further studied. “Presumably, the endothelial surface area will increase as the axial length elongates and the anterior chamber deepens if the limbal dimension does not change,” they proposed. “Because there is no mitotic activity in the corneal endothelium after birth, it is thus conceivable that the corneal endothelial cells will have to flatten to cover the enlarged surface. Subsequently, a reduced corneal endothelial density could be expected.”
Vitamin abnormalities common in neuropathic corneal pain. The role of abnormal vitamin D and B levels in various neurological conditions has previously been established. However, to date, the relationship between vitamin levels and neuropathic corneal pain (NCP), a condition characterized by abnormal nerve function, has not been studied. Researchers explored these vitamin abnormalities as a possible underlying etiology in NCP.7
“Our findings indicate that vitamin abnormalities are common in patients with NCP, specifically low B2, high B6 and low vitamin D,” the investigators wrote in their abstract. “High vitamin B6 levels was one of the most common findings, supporting literature that B6 toxicity may lead to neuropathy. Vitamin D deficiencies are more common in patients 18 to 30 years and in males.”
The retrospective study included 84 patients with NCP. Most participants (age: 40.8 years) were female (65.5%), white (77.4%) and of non-Hispanic or Latino origin (82.1%).
At least one vitamin abnormality was found in 52.4% of patients, most common being low B2 (31.0%), high B6 (28.9%), high B12 (15.0%) and low vitamin D (15.8%). Males had higher odds than females of having a vitamin D3 deficiency (OR: 4.5). The predictive value of having a vitamin D3 deficiency decreased as age increased (OR: 0.9). Specifically, patients aged 18 to 33 had higher odds of having vitamin D3 deficiency (OR: 4.89). No category of race was at greater risk for a vitamin abnormality, and no demographic group was at greater risk for a vitamin B abnormality.
“Serology testing may help treat underlying conditions early, especially in males under 33,” the team concluded. “Investigating changes in clinical findings/pain after treating abnormal levels would further illustrate the role vitamins play in NCP.”
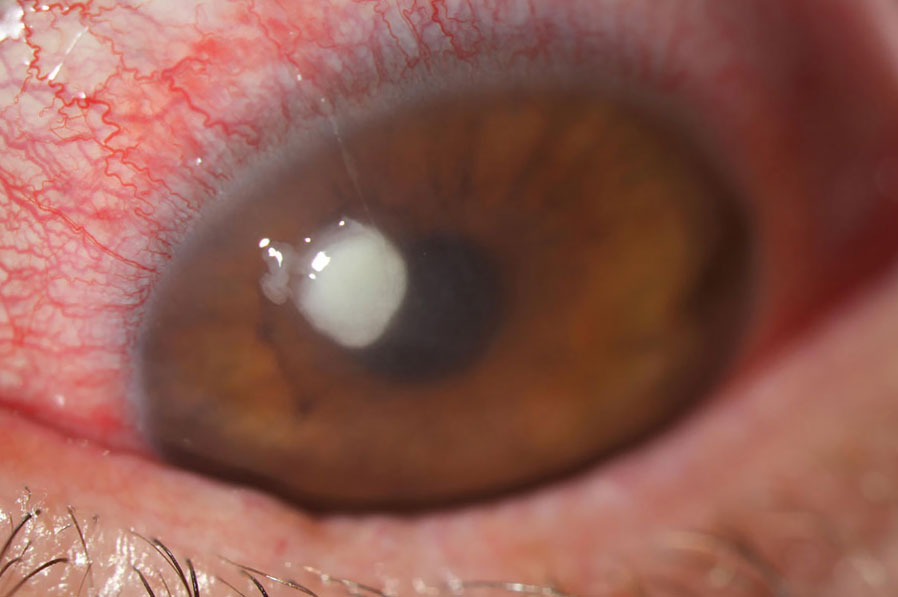
Corneal hydrops found more prevalent in younger KCN patients. A study by Cleveland-based researchers covered the lifetime prevalence of acute corneal hydrops in keratoconic eyes one-year post-treatment of corneal collagen crosslinking (CXL) or contact lenses (CLs).8
The retrospective study collected data from electronic health records to identify keratoconic patients and their initial treatment modality: either CXL or management with CLs. The primary outcome was acute corneal hydrops incidence after one year of treatment due to complications from continuing unstable keratoconus despite treatment.
Keratoconus was found in 32,141 patients. Of those, 12.1% chose to manage the condition with CLs, and 3.1% patients underwent CXL treatment. On average, CL patients were older, female and Black. Of those managed with CLs, 16 patients (0.4%) developed corneal hydrops one year after treatment compared with 10 CXL patients (1.0%). Though the aggregate numbers are small, this suggests a higher rate of hydrops development in this group.
The researchers determined that CXL patients possessed a higher absolute risk and likelihood of developing lifetime incidence of corneal hydrops. Along with this, the CL-managed group displayed greater event-free survival probability of hydrops over time relative to the CXL group. Additionally, the contact group had a lower hazard rate.
However, as Julie Song, OD, of SUNY College of Optometry, notes, the study’s results are somewhat misleading due to the age of each subgroup population. The patients managed with CLs were on average 15 years older than those in the CXL group, with average ages of 44 and 28, respectively. Keratoconic eyes tend to stabilize around age 40, she points out, which may be why hydrops prevalence was lower in the older age group. The younger CXL group was “in the age range of patients who are still susceptible to natural keratoconic progression,” which is likely a contributing factor to greater hydrops incidence, Dr. Song says. She adds that “patients who tend to undergo CXL are often patients who are already identified as having progression in their keratoconus, which is why they were referred to undergo the procedure to begin with.”
Although acute corneal hydrops is displayed here as a rare complication in both groups, the authors relay that “clinical significance remains unclear, as acute corneal hydrops represents a rare lifetime complication in both cohorts, and patients managed with CXL may be at higher risk for complications in general.”
The authors also noted that several factors must be considered when managing keratoconus, as Dr. Song echoes, and that corneal hydrops typically spontaneously resolves within two to four months along with conservative management.
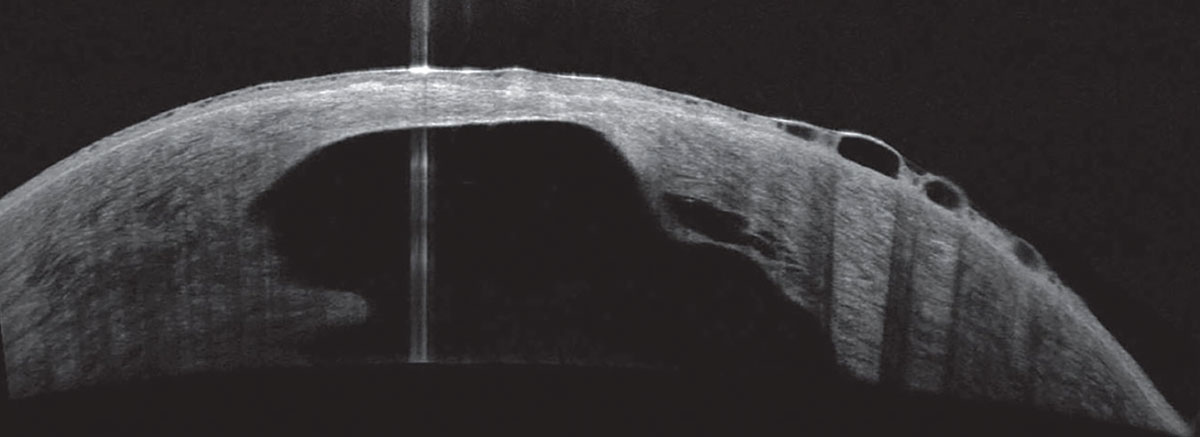 |
|
One study investigated higher rates of corneal hydrops development in keratoconus, finding it more prevalent in younger patients. Photo: Joseph Shovlin, OD. Click image to enlarge. |
Ocular Surface
Several groups of researchers presented findings of the latest studies on the treatment and management of the most common patient-reported ocular surface complaint: dry eye.
Use of several systemic meds associated with worse DED. Many systemic medications have been reported to be associated with DED, yet their associations with the severity of DED are not well studied.9 Researchers recently evaluated whether various classes of systemic medications are associated with the severity of DED signs and symptoms via secondary analysis of data from the Dry Eye Assessment and Management (DREAM) study, a large multicenter, randomized, placebo-controlled clinical trial of patients with moderate to severe DED.
A total of 535 patients with moderate to severe DED self-reported their current use of systemic medications. At baseline, six and 12 months, DED symptoms were assessed using the Ocular Surface Disease Index, and DED signs were evaluated through use of tear breakup time (TBUT), Schirmer’s test, corneal fluorescein staining, conjunctival lissamine green staining, meibomian gland dysfunction (MGD) and tear osmolarity.
Systemic medications were categorized into the following classes: statin, proton pump inhibitor, aspirin, vitamin D3, nonsteroidal anti-inflammatory drugs, steroids, diuretics and medications for treating hypothyroidism, diabetes, hypertension, seizure and migraine. Generalized linear models compared the scores of DED signs and symptoms between users and non-users of each of these medication classes, with adjustment factors that were previously found to be associated with severity of DED in the DREAM study.
Below are some notable findings among dry eye patients taking various meds compared with non-users:
- Aspirin users had lower TBUT.
- Steroid users had lower TBUT, lower Schirmer’s test scores and higher tear osmolarity.
- Seizure medication users had higher composite dry eye severity scores.
- Vitamin D3 users had lower TBUT and greater meibomian gland abnormality.
- Migraine medication users had lower Schirmer’s test scores.
- Diuretic users had less meibomian gland abnormality.
- None of the meds for systemic conditions (e.g., diabetes, hypertension) was associated with symptom severity.
The team concluded in their abstract that “use of aspirin, steroids, vitamin D3 and medications for seizure and migraine was associated with worse DED severity, while the use of diuretics was associated with less meibomian gland abnormality. No systemic medications were associated with DED symptom severity.”
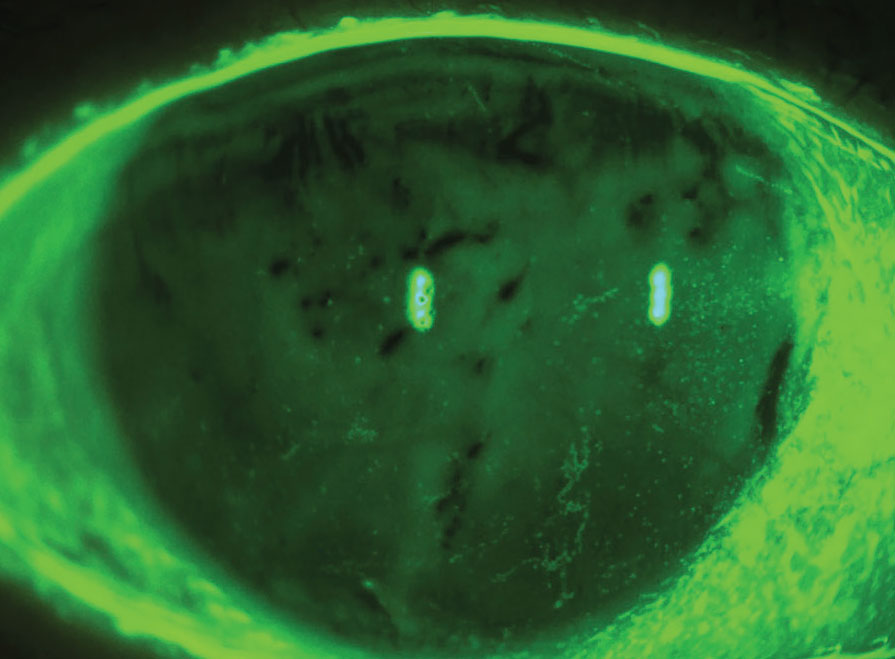
Oily skin increases risk of dry eye. It’s been proposed that meibomian lipids on the lid margin form a barrier that prevents skin lipids from entering the eye and disrupting tear film stability.10 What happens, then, when MGD upsets this balance by reducing eyelid lipid release? Optometrist Jim Kokkinakis from Sydney described his recent investigation of the interaction. Using three volunteer subjects, Dr. Kokkinakis found that applying facial lipid samples to the ocular surface caused tear film disruption, pain, fluorescein staining of the corneal surface and meibomian gland activity. According to the author, this is the first study showing the effects of skin lipid contamination of the ocular surface.
First, the side of each participant’s nose was swabbed to collect lipids found on the skin. Next, the corneal surface, eyelid margin, eyelash base or lacrimal lake were touched with either a cleaned (control) or loaded thread. Acetic acid was used as the control for low pH. Effects on the tear film were visualized using fluorescein or TearView, a new device that shows tear film formation and stability in real time.
Both TearView and fluorescein assessment showed that minimal amounts of skin lipid applied to the cornea, eyelid margin or lacrimal lake spread and destroyed the tear film’s integrity, which was not restored for several blinks. The contamination of the eye with the skin lipid sample also caused pain and staining of the corneal surface. TearView showed that introducing the skin lipid triggered meibomian lipid secretion that displaced the substance, presumably giving protection. In the control subjects, acetic acid—emulating skin pH—destroyed the tear film but did not spread from the site of touch. It caused corneal staining, and the tear film recovered with one blink. Neutral control lipids did not cause any discomfort or destroy the tear film but smeared across it during blinking. In contrast, free fatty acids had similar effects to the skin swab substance.
 |
|
The tear film may be disrupted by skin oils, which can lead to a faulty tear film and dry, irritated eyes. Photo: Pam Theriot, OD. Click image to enlarge. |
Tear film disruption is most likely due to fatty acids and low pH, which supports the proposed barrier function of meibum on the eyelid margin, the author explained. “This barrier would be compromised by diminished meibomian lipid secretion or excess of skin lipid secretion, which would overwhelm the lid margin barrier. Therefore, skin lipid contamination of the ocular surface might be a common factor for the cause of dry eye in various types of blepharitis, ocular rosacea and MGD,” Dr. Kokkinakis concluded in his abstract.
Dry eye emerges as side effect of endocrine therapy for breast cancer. Side effects such as fatigue, joint pain and stiffness are common in endocrine therapy to treat breast cancer.11 Researchers evaluated another possible side effect of this treatment: dry eye.
A total of 88 women were included in the study—56 undergoing aromatase inhibitor treatment and 32 undergoing selective estrogen receptor modulator treatment. Their ages, BMIs, treatment situations and ocular symptoms were recorded. A Comprehensive Eye Surface Detector was applied to detect patients’ ocular surface condition and evaluate for signs of dry eye. The Self-Rating Anxiety Scale and Hamilton Anxiety Scale was administered to evaluate patients’ anxiety and depression, and levels of blood lipid and sex hormone were also examined.
Seventy-seven, or 87.5%, of the breast cancer patients had dry eye. Among this group, 11.4% received selective estrogen receptor modulator treatment and 76.1% received aromatase inhibitors. The frequencies of the clinical subtypes of dry eye were evaporative dry eye (59.7%), aqueous-deficient dry eye (23.4%) and mixed dry eye (16.9%).
Among aromatase inhibitor-treated patients with dry eye, patients under the age of 50 had significantly more prevalent subjective symptoms and objective exam results of dry eye than those of patients older than 50. All breast cancer patients had different degrees of anxiety and depression, the prevalence of which were significantly higher than patients without dry eye. The degree of anxiety and depression was related to the severity of dry eye; the higher the degree of dry eye, the greater the anxiety and depression. Age, BMI, lipid profile and sex hormone level were found to not be significantly associated with dry eye.
“Taking measures to intervene in the occurrence and development of dry eye at the initial stage of endocrine treatment for breast cancer patients may greatly improve the patients’ quality of life,” the authors concluded in their abstract.
Dry eye more likely in geriatric patients with depression, anxiety. A group of researchers recently revealed an association between dry eye and the following factors: gender, age, race, geography, anxiety and depression.12 The strongest association was noted in patients with both psychiatric disorders.
The team analyzed data of 21,059 patients with clinically significant dry eye (defined as two or more dry eye claims submitted in one calendar year) from a 5% random sample of 2011 Medicare beneficiaries in the US (average age: 75). To calculate odds ratios (ORs) between dry eye and anxiety and depression, the team used logistic regression models controlled for demographical covariates.
Compared with men, women in the cohort were 2.03-times more likely to have dry eye. Patients of Asian (OR: 1.85) or Native American race (OR: 1.51) were more likely to have a diagnosis of dry eye than their white counterparts, and Black patients were even less likely to have dry eye (OR: 0.83).
 |
|
Patients with anxiety and depression may be more likely to also develop dry eye. Photo: Luis Rojas, OD. Click image to enlarge. |
Geographic residence and age also both affected ORs for dry eye; compared with patients in the Northeast, those residing in the West were more likely to have dry eye (OR: 1.38), while patients in the Northwest were less likely (OR: 0.58). Patients aged 75 and older were also more likely to have dry eye than those aged 65 to 74 (ORs: age 75 to 84, 1.49; age 85+, 1.54).
Regarding the association between depression and anxiety and dry eye, the researchers pointed out in their abstract that “having both depression and anxiety was more highly associated with dry eye (OR: 2.38) compared with having depression (OR: 1.95) or anxiety (OR: 2.22) alone.” The team concluded that “longitudinal studies evaluating the temporal relationship between dry eye and psychiatric disease are warranted.”
DREAM study researchers again challenge omega-3 efficacy in DED treatment. Several studies have investigated the potential benefit of omega-3 fatty acid supplementation in the treatment of DED. However, to date, such literature—including the widely reported DREAM study—has not provided convincing evidence that omega-3 fatty acids are effective in controlling DED symptoms or progression; rather, the pills showed results similar to the placebo.13
While the original DREAM study only followed patients for 12 months, researchers—again led by study chair Penny Asbell, MD—recently obtained an additional year of data from moderate to severe DED patients who had been initially randomized to receive omega-3 pills the first year. During the second year, these participants (n=43) were re-randomized to either continue with omega-3 (n=22) or switch to placebo (n=21). The team evaluated the progression of DED symptoms and signs over the two years with follow-ups at baseline, three, six, 12, 18 and 24 months.
The data showed that at three months, DED patients taking omega-3 showed significant improvements in Ocular Surface Disease Index and Brief Ocular Discomfort Index scores and less use of artificial tears or gel; however, after this period (an additional six to 24 months), DED symptoms and treatments remained stable. There were also no significant changes over two years in corneal staining, TBUT, Schirmer’s test, MGD, tear osmolarity or noninvasive keratography measures in patients treated with omega-3. The only DED metric that did show a significant change in the treatment group over two years was conjunctival staining score.
The researchers explained in their abstract that the significant improvement in subjective DED symptoms in the first three months of omega-3 treatment could be chalked up to a placebo effect or regression to the mean. Due to this observation, they noted that “future clinical trials of DED should consider the short-term placebo effect of treatments on DED symptoms.”
The results of this randomized follow-up study on the DREAM cohort suggest that omega-3 supplementation and observation promote comparable treatment outcomes over two years in DED patients. Additionally, the researchers concluded in their abstract that “these results do not support progression of DED over the two years of observation.”
Contact Lenses
Let’s take a closer look at some of the studies presented on this ever-evolving area of eye care.
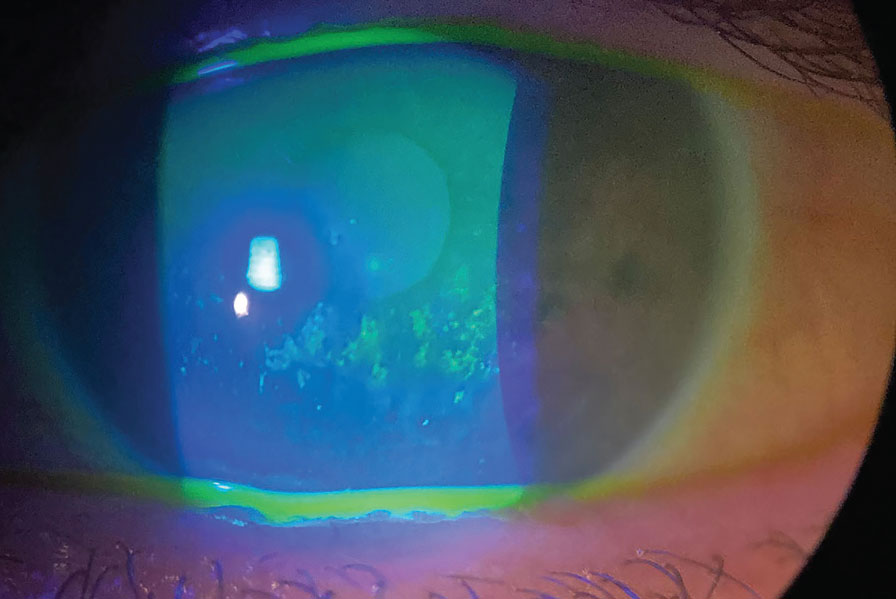
Myopia control with soft multifocals benefits all progression rates. Two presentations evaluated reports from the BLINK (Bifocal Lenses in Nearsighted Kids) study on multifocal CL myopia control. The first one compared myopia progression and axial elongation in children wearing +2.50D add multifocal vs. single-vision CLs to find out whether the treatment effect of optical myopia control is better for fast progressors, and results suggest that children receive a similar amount of treatment benefit from myopia control regardless of their underlying rate of progression.14
The BLINK study randomized 294 children between the ages of seven and 11 to wear Biofinity soft CLs for three years in either a D-design with a +2.50D add, +1.50D add (not analyzed in this study) or single-vision CLs. Cycloplegic refractive error was between -0.75D to -5.00D (sphere, inclusive) at baseline with less than 1.00D of astigmatism. Three-year myopia progression and axial elongation for single vision (n=96) and +2.50D add (n=95) groups were plotted against their cumulative frequency Z-scores with slopes estimated by linear regression.
Differences between treated and control groups only varied by ±0.11D across two standard deviations of myopia progression with no significant variation across the range of axial elongation. The variations were not large enough to create meaningful differences between the treated and control groups over three years. “A uniform treatment benefit suggests that all children should be considered candidates for optical myopia control rather than prioritizing those at risk for fast progression,” the authors concluded in their abstract.
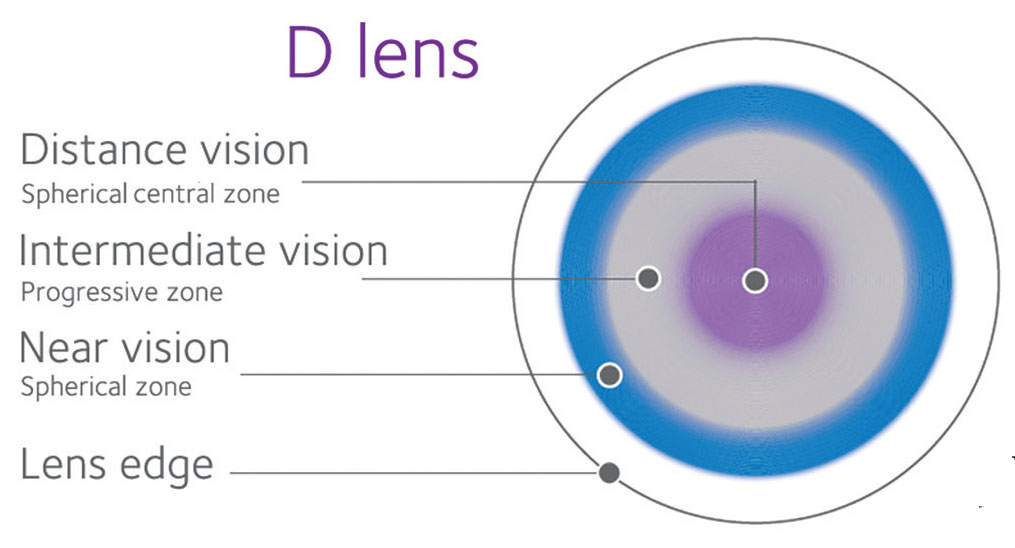 |
|
Results from the BLINK study suggest that treatment effect for myopia control is similar for all progression rates in children and that soft multifocal CLs don’t affect comfort, focus or how well the two eyes work together. Photo: CooperVision. Click image to enlarge. |
The second presentation compared Convergence Insufficiency Symptom Survey findings, phoria and accommodative lag between single-vision and multifocal CL wearers with +1.50D add and +2.50D add over three years and found that myopia control with soft multifocal CLs does not negatively affect how well the two eyes work together, how accurately they focus on a near target or the comfort of the eyes.15
The accommodative lag was less than baseline at all visits for the three groups, except the lag was similar between baseline and two weeks for +2.50D add. The only differences observed were between single vision and +2.50D add at two weeks and one year and between single vision and +1.50D at two weeks. The maximum difference between groups in average accommodative lag was never more than 0.33D. Near phoria was statistically significantly more exophoric after baseline for both add powers but never became more than 2.40 prism diopters more exophoric over the three years. The +2.50D add group was more exophoric than the single-vision group at all visits after baseline but never more than 2.00 prism diopters more exophoric on average over three years.
Take note of subjective vision with teens in myopia control contacts. The optics of myopia control soft CLs slow myopia progression, but they can also reduce vision quality vs. conventional optical designs. Myopia control soft CLs are often evaluated in younger children (≤12), but meaningful myopia progression can occur during their teen years. Researchers at Johnson & Johnson Vision performed a post-hoc analysis of a prospective clinical study in myopic children (ages seven to 17) that assessed subjective vision with myopia control soft CLs using a patient-reported outcomes questionnaire.16 They found that older children were more judgmental of their vision experience during early wear.
The team conducted a multi-site, single-masked, 3x3 crossover study with a run-in period. Healthy myopic children aged seven to 17 years old were recruited, balancing the number of children seven to 12 with those 13 to 17. Subjects initially used a daily disposable soft CL with conventional optics for one week, then lens wear sequence was randomized and subjects were fit with one of three myopia control soft CLs for three two-week periods. There were two senofilcon A prototype myopia control soft lenses with noncoaxial ring-focus designs (for enhancing efficacy and enhancing vision) and one omafilcon A dual-focus design. Subjective vision was assessed using the Pediatric Myopia Control Questionnaire at the two-week follow-up. An overall vision item was analyzed using the Pearson chi-square test to assess differences in top two box score proportions between the two age groups (excellent and very good) for each lens type separately.
The intent-to-treat population included 75 participants, with 38 aged seven to 12 (mean age: 10.6) and 37 aged 13 to 17 (mean age: 14.7). The researchers detected a significant difference in top two box score proportions by age for enhancing efficacy and approach for dual focus, but there was no significant difference for conventional optics or enhancing vision.
“A different balance of vision quality and myopia control efficacy may be prudent in older children to better fit their more critical assessment of vision quality and decrease the average annual myopia progression rate,” the researchers concluded in their abstract.
These informative findings will help ODs devise new ways to help their patients. Check out ARVO’s full listing of abstracts and posters to see for yourself the latest advances in eye and vision care.
1. Sanfilippo CM, DeCory H, Asbell PA. Antibiotic resistance among ocular pathogens – an update from the 2022 ARMOR Study. ARVO 2023 annual meeting. 2. Asbell PA, Sanfilippo CM, DeCory H. Longitudinal analysis of in vitro antibiotic resistance rates among ocular staphylococci collected in the ARMOR Study. ARVO 2023 annual meeting. 3. Maretz C, Atlas J, Shah S, Wozniak R. Infectious keratitis treatment failure—a study of patient and microbial characteristics in Rochester, NY. ARVO 2023 annual meeting. 4. Lieberum J, Zander D, Reinhard T, et al. Lifestyle risk factors across Fuch’s endothelial corneal dystrophy severity. ARVO 2023 annual meeting. 5. Bernal A, Yang Y, Surenkhuu B, et al. Corneal epithelial thickness in dry eye disease (DED) patients: association with autoimmunity. ARVO 2023 annual meeting. 6. Chalkiadaki E, Tsiripidis K, Gartaganis P, et al. Correlations of corneal endothelial morphology with anterior segment parameters in healthy adults. ARVO 2023 annual meeting. 7. Bogen CS, Cox S, Hamrah P. Role of vitamin abnormalities as possible underlying etiology in patients with neuropathic corneal pain. ARVO 2023 annual meeting. 8. Nguyen C, Siso D, Truong N, et al. Lifetime incidence of corneal hydrops in keratoconic eyes post corneal collagen crosslinking vs. contact lens management. ARVO 2023 annual meeting. 9. Guo M, Patel C, Yu Y, et al. Association between systemic medication use and severity of dry eye symptoms and signs in the DREAM study. ARVO 2023 annual meeting. 10. Kokkinakis J. In vivo evidence that skin lipids may be a cause of dry eye in humans. ARVO 2023 annual meeting. 11. Ma N, Zhang C, Zhao H. Dry eye, its clinical subtypes and associated factors in breast cancer patients undergoing endocrine therapy: a cross-sectional study. ARVO 2023 annual meeting. 12. Li G, Vargas CG, Klawe J, et al. Association of dry eye with demographic characteristics, geography, and psychiatric comorbidity in the geriatric population. ARVO 2023 annual meeting. 13. Daniel Lee D, Yu Y, Bunya VY, et al. Two-year progression of dry eye disease in the dry eye assessment and management (DREAM) study. ARVO 2023 annual meeting. 14. Mutti DO, Sinnott LT, Berntsen DA, et al. Uniformity of treatment benefit in multifocal contact lens myopia control. ARVO 2023 annual meeting. 15. Walline JJ, Tomiyama E, Sinnott LT, et al. Phoria, accommodative lag and symptoms of soft multifocal contact lens myopia control. ARVO 2023 annual meeting. 16. Nixon A, Xu J, Brennan NA, et al. Subjective vision differences with soft contact lenses for myopia control in children and teenagers. ARVO 2023 annual meeting. |


