Each year, the Association for Research in Vision and Ophthalmology (ARVO) annual meeting gifts the eyecare profession with a cornucopia of new research that lets us see where the winds are blowing clinically. Here, we’ve compiled research specific to cornea and contact lens care we feel may be most impactful for practicing optometrists.
This year’s meeting was held in Seattle from May 5-9. The theme of ARVO 2024 was “imagining innovation and intelligence in vision science.” Vision research is continually being transformed by new information and technologies. The findings summarized here are only a snippet of those presented at the meeting, of course, but show the rich expanse of insights ARVO generates each year.
Cornea
This year’s presenters highlighted a host of exciting research from the last 12 months focused on this part of the eye.
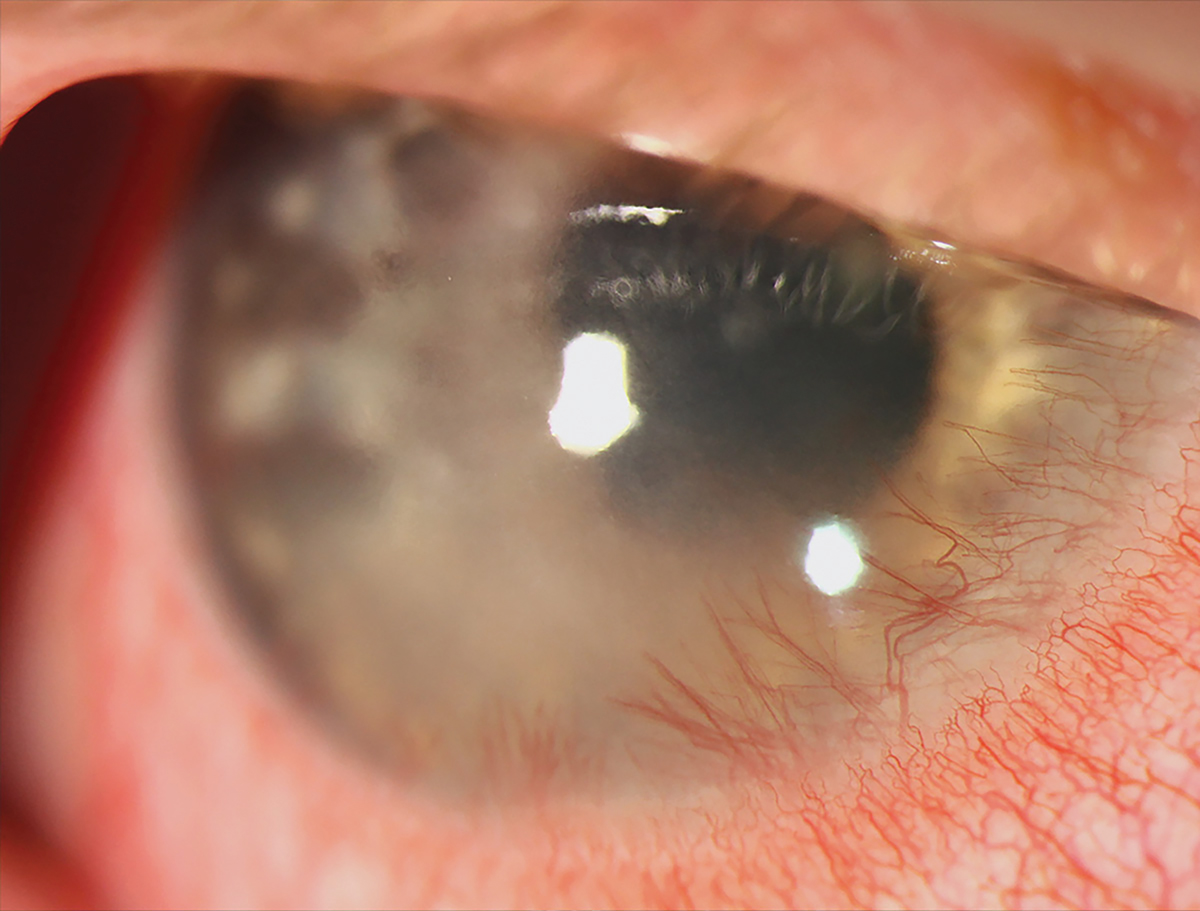
Corneal complications common in peds patients with herpetic keratoconjunctivitis (HKC). Pediatric ocular surface inflammatory diseases can greatly impact the vision and quality of life of these young patients, but limited data has been presented on the three most common forms—blepharokeratoconjunctivitis (BKC), HKC and vernal keratoconjunctivitis (VKC). Researchers investigated the clinical features and practice patterns of these conditions using a real world data asset with de-identified administrative claims and electronic health record data.1
A total of 6,116 patients aged 18 years and younger over a one-year span were included. Clinical information from six months before to three years following the clinical appointment (index date) was analyzed.
Corneal complications were more prominent in HKC, while high-potency corticosteroid use was more common in those with BKC. The limited use of topical immunomodulators suggests the potential for improving treatment approaches.
“Up to the index date, blepharitis was observed in 5.3%, with higher rates in BKC (13.5%) than HKC (4.9%) and VKC (3.6%),” the researchers explained in their abstract. Giant papillary conjunctivitis was found in 10.4% of BKC, 11.3% of VKC and only 3.6% of HKC cases. Corneal scarring and ulceration rates were significantly higher in HKC compared to BKC and VKC both before and after the index date.
“Antivirals were more common in HKC cases,” the authors continued. “Surgical interventions for complications were uncommon, with corneal perforations limited to BKC cases.”
 |
|
Be mindful of elevated corneal scarring risks in pediatric HKC patients, new research advises. Photo: Alison Bozung, OD. Click image to enlarge. |
Insulin eye drops may aid corneal healing. In two posters presented at ARVO 2024, a new possible treatment was investigated for corneal wounds. The first was a retrospective review of patients with neurotrophic keratitis resistant to conventional treatment, while the second study dealt with neurotrophic corneal ulcers. Re-epithelialization was faster and more successful with the treatment vs. conventional methods.
In the first study, patients between ages 55 and 69 were classified into two groups: Group I received topical insulin therapy with 4 units per mL of concentration and Group II received conventional treatment. Of the 52 patients included (52 eyes), 27 eyes were designated to Group I and 25 to Group II.2
Mean time between diagnosis and start of treatment was longer in Group I than Group II, and no differences were seen in baseline characteristics between the two groups. Re-epithelialization was achieved in 74% of Group I (20 eyes) and 64% in Group II (16 eyes). Mean time to re-epithelialization was also shorter in Group I than Group II (32.3 days and 82.5 days, respectively). Final defect area was smaller in the insulin group as well, but no significant differences were seen between groups in visual acuity. There were also no observed differences in recurrences, complications and subsequent surgical interventions.
The study authors reason, “the use of insulin aims to support nerve regeneration and enhance the overall repair process in the affected eye. This approach holds potential for improving the outcomes and management of neurotrophic keratitis.”2
Similarly, the second study also used insulin drops for treatment of refractory neurotrophic corneal ulcers in vivo and investigated cellular mechanisms underlying re-epithelialization of corneal epithelial wounds in vitro. Included were patients with the condition treated with topical insulin eye drops; corneal epithelial wound closure was monitored daily. As well, human primary limbal epithelial cells were incubated in serum-free medium either with or without different insulin concentrations, ranging from 0.05µg/mL to 150µg/mL, for 24 hours.3
The researchers observed that all 20 eyes achieved complete corneal re-epithelialization after insulin standard treatment regimens (25U/mL or 0.5U/drop). However, outcomes were not enhanced by higher doses, instead appearing to induce corneal angiogenesis. A significant dose-dependent effect of insulin on epithelial migration was most effective with lower doses (0.5µg/mL to 1.0µg/mL). Upregulation of genes FSCN2 and TSPAN1 was found, both of which are involved in cell migration. Conversely, downregulation was seen with cell adhesion molecules, including integrin subunits, after exposure to 1.0µg/mL to 5.0µg/mL of insulin. Even greater insulin doses (50µg/mL to 100µg/mL) induced a 2.5-fold upregulation of vascular endothelial growth factor A.3
In both studies, topical insulin treatment is not yet available, but they display the possible benefits and prospects for its future use.
Corneal edema post-cataract more common in diabetics. While cataract and refractive surgical procedures have evolved tremendously in recent decades, postoperative corneal edema is still commonly present. Researchers at the Icahn School of Medicine at Mount Sinai in New York City studied which factors increase the risk of developing corneal swelling and which patients eventually required corneal transplantation after cataract surgery. Their study demonstrated that people with diabetes were more likely to have corneal edema after surgery. Older individuals also had a higher risk, and this risk increased with age. Notably, different racial and ethnic groups had a higher likelihood of developing corneal edema and needing a corneal transplant compared with Caucasian patients.4
The researchers collected data from a nationwide sample of 192,150 Medicare beneficiaries 65 years old and older who received cataract surgery. Patients with diabetes were more likely to develop corneal edema compared with non-diabetic patients after cataract surgery (odds ratio [OR]: 1.25). Compared with patients aged 65 to 74, patients aged 75 to 84 (OR: 1.38) and over 85 (OR: 2.40) were more likely to develop corneal edema. Compared with Caucasian patients, Black, Asian, Hispanic and North American Native patients were significantly more likely to develop both corneal edema and eventually require corneal transplantation. Female patients had lower odds of requiring corneal transplantation postoperatively (OR: 0.53).
In these patients, the presence of macular edema was associated with increased odds of developing corneal edema (OR: 1.86). However, the researchers found that the severity of diabetic retinopathy, diabetic kidney disease and the presence of peripheral circulatory disease were not associated with increased odds of corneal edema.
 |
|
In those with CXL treatment failure, the mean time to a repeat CXL, DALK or PK procedure was 182 days. Photo: Lily Arendt, OD. Click image to enlarge. |
Humidity may be a risk factor for keratoconus. The progressive changes wrought by keratoconus, if left unchecked, can be devastating, leading to distorted vision and visual impairment. Researchers are curious about what factors may affect its development. Given the wide variance by ethnicity, there is a genetic component at work. At ARVO, one group of researchers presented their results detailing climate-related variables and their relation to the condition. The group systematically reviewed studies on keratoconus prevalence and incidence in the general population. Climate datasets like the ERA5 as well as its derivatives were used to find data for each studied region. The climate exposure period consisted of the 10 years preceding data collection for each prevalence study. Averages of relative humidity, wind speed, ultraviolet radiation and maximum daily temperature were calculated over this period.5
Included were 18 total systematic reviews reporting prevalence of keratoconus across different geographical locations. In the multiple regression model, only humidity and keratoconus prevalence yielded a negative association; maximum daily temperature, wind speed and ultraviolet radiation did not display significant associations with prevalence of the condition.
The authors subsequently pose that “low humidity might therefore be an unexplored risk factor for keratoconus,” they noted in their ARVO abstract. “Further research is needed to investigate the importance of humidity for the cornea and to assess whether humidification might have preventive and therapeutic applications.”
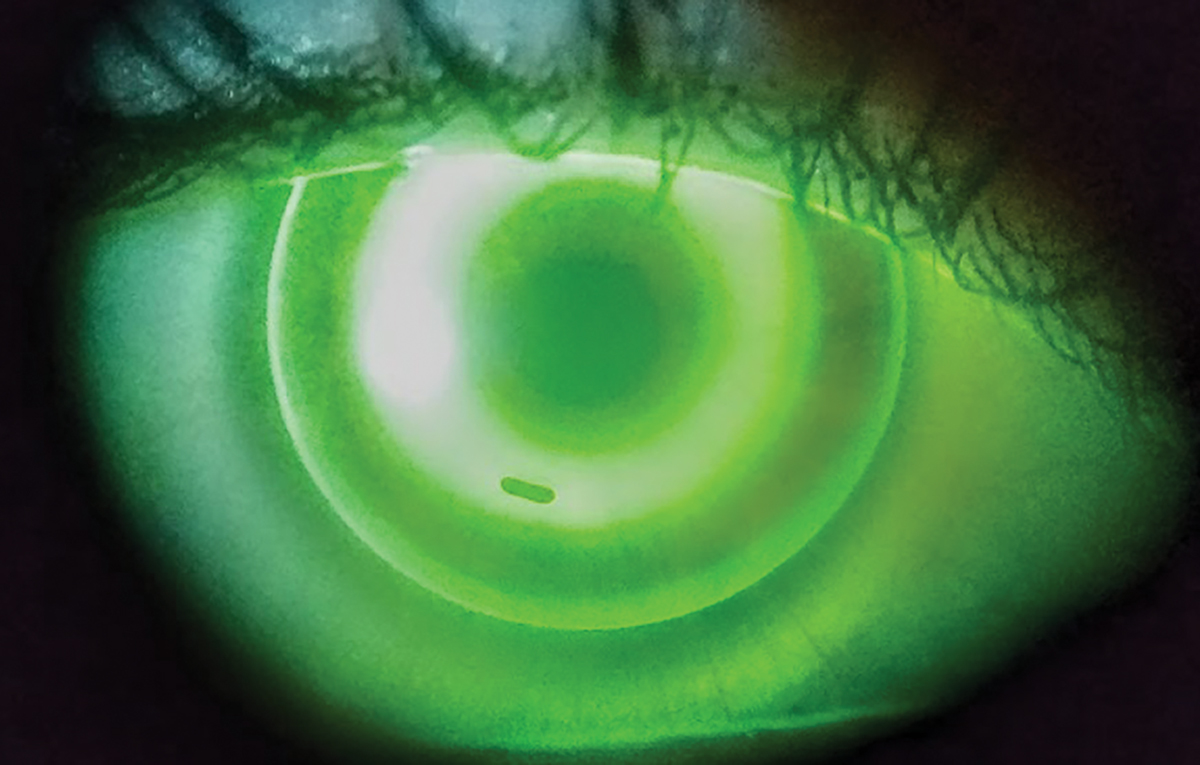
Allergies, atopic disease linked to higher crosslinking (CXL) failure rate. For keratoconus suspects and patients, asking pertinent questions about a history of eczema, asthma, allergy and eye rubbing should be part of the entering case history. A study presented reinforced the necessity of this step, as it determined that allergy and topic disease were associated with a higher treatment failure rate of corneal CXL.6
Researchers from Wills Eye Hospital in Philadelphia conducted a retrospective claims-based analysis of patients from a 15-year period. They excluded patients who had enrollment beginning less than one year before initial CXL and patients who had undergone previous penetrating keratoplasty (PK) or deep anterior lamellar keratoplasty (DALK). The primary study outcome was time to treatment failure repeat CXL, PK or DALK identified by CPT-4 codes. The analysis involved 3,107 eyes from 2,356 patients with keratoconus who underwent CXL. Mean age was 31.8 years, and 67.5% of patients were male. Mean enrollment length was 4.6 years, and 1.2% of eyes (n=37) from 35 patients experienced treatment failure. Of this group, 31 underwent a repeat CXL. The mean time to repeat CXL, DALK or PK was 182 days.
The researchers noted that CXL failure was more likely to occur in patients with allergic or atopic disease (56.8% vs. 40.0%). There was no difference in failure rates by pediatric status (18.9% vs. 12.9%), sleep apnea (21.6% vs. 14.8%) or sex (40.5% vs. 33.2% female).
“Our study characterized rates of corneal CXL failure in patients with keratoconus using a large insurance claims database,” they emphasized in their ARVO abstract.
 |
|
After ortho-K treatment, eyes in the 5mm optic zone group had a smaller treatment zone, although there was no difference in decentration. Photo: Dan Fuller, Od. Click image to enlarge. |
Contact Lenses
Let’s take a closer look at some of the studies presented on this ever-evolving area of eye care.
No meaningful rebound effect seen after discontinuing multifocals for myopia control. In late 2019, the Bifocal Lenses in Nearsighted Kids (BLINK) Study found that +2.50 add center-distance multifocal contact lenses slowed eye growth and myopia progression compared with single vision contact lenses or +1.50 multifocal lenses. At ARVO 2024, the research team presented the results of BLINK2, in which “the same children all wore the high-add multifocal for two years and then were changed to single vision contact lenses for the last year to determine if eye growth returns to a normal rate or if there is an acceleration of eye growth faster than expected for their age (i.e., rebound),” says lead author of the ARVO paper and one of the principal investigators of the BLINK study, David A. Berntsen, OD, PhD, of the University of Houston.
BLINK2 included 248 (59% female) myopic children between the ages of 11 and 17 (mean age: 14.9). Axial length (AL) was measured every six months using optical biometry and spherical equivalent refraction (SER) was measured annually by cycloplegic autorefraction. While there was a statistically significant increase in eye growth and myopia progression after discontinuing multifocal contact lens wear, the increases were small and not clinically meaningful.7
“We did not find evidence of a rebound or faster than normal eye growth, at least when you wait until children are older like they were in BLINK2,” Dr. Berntsen explains.
After all participants switched from multifocals to single vision lenses at year two, there was an increase in AL growth of 0.04mm/year that did not depend on the original BLINK treatment assignment. For SER, there was also an increase in myopia progression (-0.16D/year) after switching from multifocals to single vision lenses at year two that also did not depend on the original BLINK treatment assignment. There continued to be a difference in AL and SER throughout BLINK2 based on the BLINK Study treatment assignment.
“Knowing that we did not find evidence of a rebound after discontinuing multifocal contact lens wear is helpful because the effect needs to remain after discontinuing treatment,” Dr. Berntsen says. “Our results provide evidence for eyecare providers that if they wait until the late teen years, they should not expect a rebound effect when discontinuing myopia control contact lenses.”
The most surprising result the researchers noted, according to Dr. Berntsen, is described not in the ARVO presentation but in a recently published research paper looking at whether defocus explains the high add multifocal treatment effect. “We did not find evidence that retinal defocus does a good job of explaining which children will benefit most from wearing a multifocal contact lens. This means there must be something else caused by the optics of the contact lens that signals to the eye to slow growth when wearing a multifocal,” says Dr. Berntsen. “More work is needed to understand the mechanism behind the treatment effect so we can optimize treatments.”
Smaller back optic zone diameter improves ortho-K results. Overnight wear of orthokeratology (ortho-K) lenses elicits a flattening of the central portion of the cornea as well as a steepening of its peripheral portion. The flattened central portion of the cornea improves daytime vision, while the steepened peripheral causes a relative corneal refractive power shift from the baseline, leading to myopic defocus on the peripheral retina. Many researchers have suggested this as the underlying mechanism of slowing AL growth. A recent study presented highlighted that a smaller back optic zone diameter (BOZD) in an ortho-K lens was associated with a greater accumulation of relative corneal refraction power shift in the central 4mm area.8
The prospective study involved a collaboration between Tianjin Eye Hospital in China and Nova Southeastern University in Fort Lauderdale, FL. In 34 children (14 boys and 20 girls; ages nine to 12), one eye was randomly assigned to wear a 5mm BOZD lens and the other eye a 6mm BOZD lens. Evaluation visits were scheduled at baseline, one day, one week, one month, three, six, nine and 12 months after the initial lens wearing.
At baseline, there was no difference in refractive error (-2.52D vs. -2.45D) or axial length (24.50mm vs. 24.50mm) for eyes wearing lenses of different BOZDs. After treatment, eyes in the 5mm optic zone group had a smaller treatment zone (6.63mm2 vs. 8.11mm2), although there was no difference in decentration. Axial length growth was significantly smaller for eyes in the 5mm optic zone group (0.19mm vs. 0.26mm). Significantly greater relative corneal refraction power shift accumulated within the central 4mm area (15.54D*mm2 vs. 10.40D*mm2) was also observed in participants wearing 5mm lenses. Relative corneal refraction power shift was significantly associated with axial length growth.
“Children wearing ortho-K lenses with smaller BOZD showed much smaller AL growth,” the researchers concluded in their abstract.
Ocular Surface
Several groups of researchers presented findings of the latest studies on the treatment and management of the most common patient-reported ocular surface complaint: dry eye.
First specific genetic locus detected for dry eye. Dry eye disease (DED) has been somewhat difficult to phenotype, in turn, limiting the application of large-scale genome-wide association studies (GWAS). One group of researchers used the VA Million Veteran Program biobank to study the genetic basis of DED.9
The authors created a case-control algorithm based on ICD-9/10 codes and prescription records, which was then reviewed and validated manually with a chart at different VA eye clinics. When the algorithm was used in this particular biobank, it detected 48,794 cases of DED and 29,224 controls. From there, the researchers classified cases into ancestry groups (European, African, Hispanic and East Asian).
After compiling this data, the researchers saw that their chart review revealed a positive predictive value of 98% and a negative predictive value of 93%. DED was found to be associated with factors of female sex, age, African ancestry and score on the Charlson Comorbidity Index, a measure of the relative one-year risk of mortality based on 17 possible comorbid conditions. They also found specific associations with comorbidities of depression and sleep apnea.
“In addition to identifying the first GWAS locus for DED, we attained a significant overall genetic signal, motivating expanded GWAS
meta-analyses and the development of polygenic risk score models.” For clinicians, this provides new insights into the genetic basis of DED and sheds light on underlying causes.
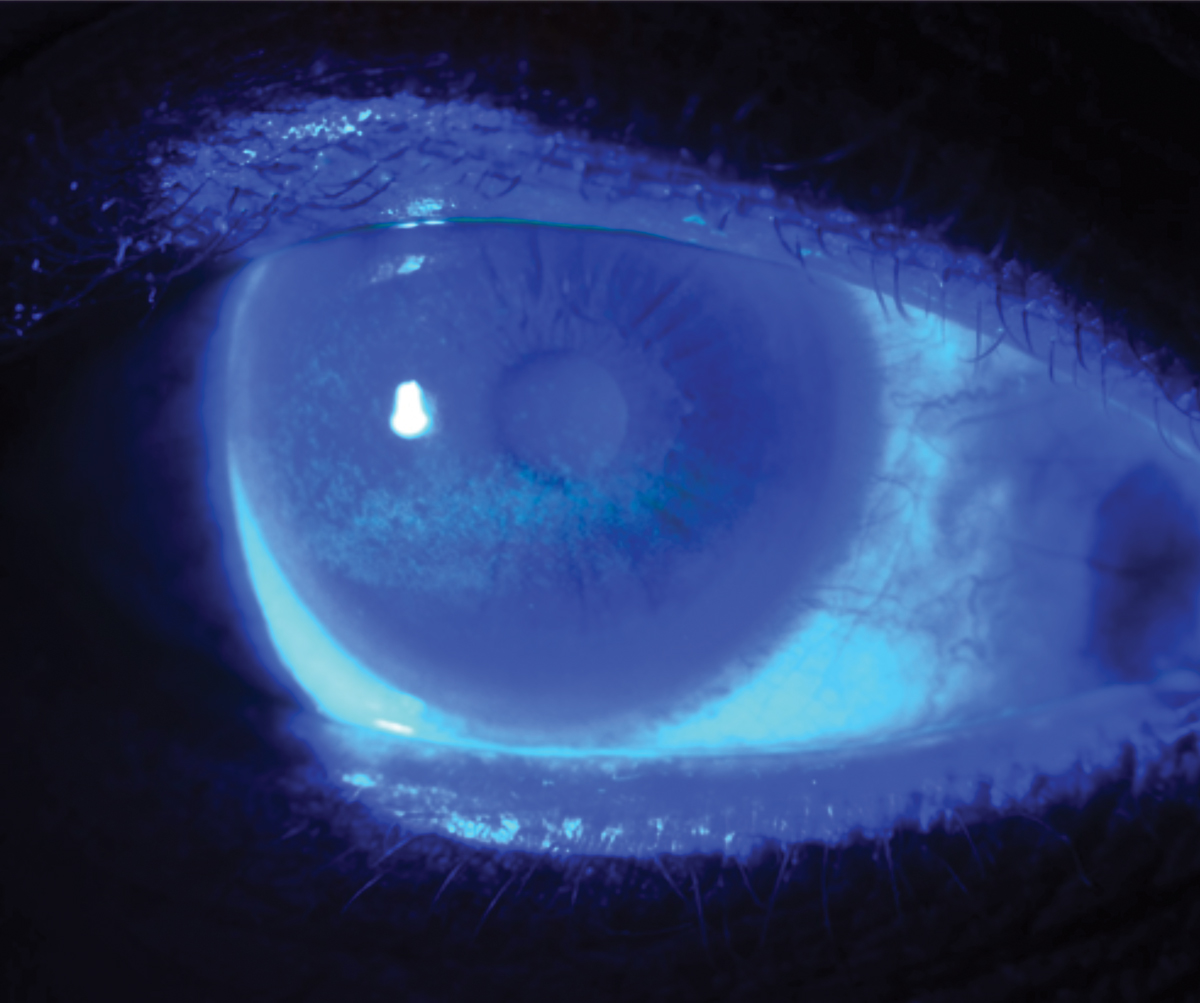
DREAM Study cohort shows dry eye test repeatability needs improvement. Clinicians have several tools at their disposal for diagnosing and monitoring patients’ DED, but experts note that there’s no single gold standard test. Also worrisome is the variable repeatability of many such tests. At ARVO, DREAM Study researchers reported retrospective findings on dry eye test repeatability, an indication of a test’s reliability as a diagnostic tool. They focused on eyes with moderate to severe disease. In the moderate to severe patient population, they found only moderate test repeatability.10
The randomized DREAM study included a screening visit and a baseline visit about two weeks apart. At both visits, DED was assessed by the same physician in the same order: tear break-up time (TBUT), corneal fluorescein staining, meibomian gland dysfunction (MGD), conjunctival lissamine staining and Schirmer test.
The researchers of the present study calculated the agreement of dry eye signs for 1,046 eyes (523 patients) between the two visits. They reported variable measurement agreement between visits. Corneal staining score had the least variability, followed by conjunctival staining score. These were followed by Schirmer test, MGD and TBUT, respectively.
A substantial percent of eyes showed clinically significant absolute differences between visits, with two or more points in conjunctival staining score in 17.8% of eyes, three or more points in corneal staining score in 9.9% of eyes, three or more seconds of TBUT in 6.2% of eyes, 5mm/5 min or greater in 22.7% of eyes for Schirmer test and greater than two points in 13.7% of eyes for MGD.
“These findings suggest the need to consider test-retest variability of DED measurements when designing dry eye clinical trials and monitoring disease progression,” the researchers concluded.
Maximum blink interval helps detect dry eye cases with mismatch of signs vs. symptoms. It is confounding in dry eye care when patients’ signs and symptoms don’t align, with one or the other factor out of proportion based on what would be expected. To better observe and assess dry eye cases with such discrepancies, researchers from Japan evaluated the maximum blink interval—or duration someone can keep their eyes open before blinking—in patients without a history of cataract surgery.11
A total of 364 patients were examined to determine whether they had positive or negative dry eye symptoms (DES) according to the Japanese version of the Ocular Surface Disease Index (OSDI) as well as positive or negative corneal epithelial damage (CED) after finding the patients’ corneal fluorescein staining score.
Participants were divided into two groups (presence or absence of discrepancy), then split again into four subgroups. The discrepancy groups separated patients into these subgroups:
- symptoms (+), signs (-)
- symptoms (-), signs (+)
Subjects with no discrepancy either had both symptoms and signs together or neither of those findings.
The maximum blink interval results for the “symptoms but no signs” group were significantly shorter compared to the “no symptoms, no signs” group (10.9 sec. vs. 14.6 sec). Also, the group with signs but not symptoms achieved a significantly longer maximum blink interval than the group with both (12.2 sec vs. 9.6 sec).
The researchers did two more subgroup comparisons: symptomatic vs. asymptomatic patients without signs and the same symptomatic vs. asymptomatic comparison in those with signs. They found a significant association between maximum blink interval and symptom/finding discrepancy for each pair of groups. Researchers did not find any significant differences between TBUT and tear secretion volume.
“Maximum blink interval may be able to evaluate cases with high symptoms-to-findings discrepancy that cannot be well-assessed using traditional diagnostic strategies,” explain the researchers in their study. “Our findings suggest a potential usefulness of these interval measurements in identifying atypical dry eye cases, where patients have prominent corneal findings but no symptoms.”
 |
|
Variability in testing can make it more challenging for clinicians to accurately diagnose and interpret changes in dry eye signs and symptoms. Photo: W.R. Buie, OD. Click image to enlarge. |
Artificial tears effectiveness comparison. A limited number of studies have compared the performance of different OTC drops for DED, prompting researchers to conduct a new study evaluating the effectiveness of 13 artificial tear preparations in improving objective measures of tear film anatomy and function in patients with dry eye. The results indicated that no artificial tear excelled across the board, so tailoring specific drops to patients with certain aspects of DED dysfunction may be beneficial.12
The study included 242 eyes from 122 patients. Tear meniscus height, noninvasive keratographic tear breakup time (NIKBUT) and central lipid layer thickness were measured using advanced keratography and interferometry. The artificial tear formulations tested included Systane Complete PF, Refresh Relieva, GenTeal Gel, Hylo-Tear, Ivizia, Systane Ultra, Refresh Optive Mega 3, Similasan, Soothe XP, Up&Up, Visine and GenTeal Tears. Saline was used as a control.
While all artificial tear preparations resulted in an improvement in some tear parameters, no single artificial tear performed consistently better at all time points for all measures. The best performer for tear meniscus height was GenTeal Gel; for NIKBUT, the winners were Systane Ultra, saline and Refresh Relieva. The most improvement in lipid layer thickness was seen with Hylo-Tear and Soothe XP. These findings suggest that the composition of artificial tears plays a crucial role in their relative performance.
High BMI a risk factor for dry eye symptoms in children. Researchers from the Illinois Eye Institute found that high BMI is a significant risk factor for dry eye symptoms in children between the ages of five and 18. A total of 160 children (76 boys, 84 girls from ages 5 to <18) underwent a comprehensive eye exam and were surveyed regarding electronic screen time and filled out a modified, child-friendly OSDI. The second OSDI question (eyes that feel gritty) was modified to “eyes that feel something inside.” The seventh OSDI question (driving at night) was removed based on the age of the study population and the eighth OSDI question (working with a computer or bank machine) was modified to “using an iPad or tablet.” Parents were surveyed on their child’s screen time, diet and outdoor activity. BMI was calculated using measured height and weight.13
High BMI was a significant risk factor for dry eye symptoms in children aged five to <18 years; however, the OSDI score was not associated with age, race, gender, screen time, outdoor activities and diet.
The mean OSDI score was 14.7, with 16.9%, 8.8% and 12.5% of the children having mild, moderate and severe dry eye symptoms, respectively. Average screen time per week was 9.2 and 8.5 hours reported by children and parents, respectively. Significant correlation was found between the screen time reported by children and parents.
“Our studies suggest that dry eye disease is frequently underdiagnosed in pediatric patients. In our data analysis, multiple regression showed that high BMI was a significant risk factor for dry eye symptoms in children; however, the OSDI was not associated with age, race, gender, screen time, outdoor activities or diet,” says Lindsay Sicks, OD, of the Illinois Eye Institute, one of the researchers. There is mixed literature on the connection between BMI and dry eye and meibomian gland dysfunction in adults, and even less evidence in children, she points out. “We wanted to investigate this association among our clinic population, which is primarily African American and Hispanic.”
Dr. Sicks notes the mechanism connecting BMI to dry eye is unclear at this time. “There are a lot of other facets to dry eye,” she explains. “In a separate analysis of this cohort (forthcoming OVS publication, Fall 2024), we found evidence that BMI is correlated to meibomian gland morphological changes (atrophy and tortuosity) as well as survey information collected about diet.” More analysis is needed to link the signs to the symptoms and to assess the relationship between all of these variables, Dr. Sicks stresses. “Still, I don’t think we can extrapolate what we find in our particular pediatric population to the general adult population at this point,” she adds.
These informative findings will help ODs devise new ways to help their patients. Check out ARVO’s full listing of abstracts and posters to see for yourself the latest advances in eye and vision care.
1. Boghosian T, Perez C, Coleman A, et al. Pediatric ocular surface inflammatory diseases (POSID): clinical feature and practice patterns. ARVO 2024 annual meeting. 2. Graue-Hernandez EO, Anaya-Barragan F, Vera-Duarte GR, et al. Topical insulin for persistent corneal epithelial defects in neurotrophic keratopathy. ARVO 2024 annual meeting. 3. Zeisberg VEB, Zenkel M, Gießl A, et al. Insulin for treatment of neurotrophic ulcers: clinical evidence and potential mechanism. ARVO 2024 annual meeting. 4. Li G, Sommi A, Klawe J, Ahmad S. Risk factors for corneal decompensation in diabetic and non-diabetic patients after cataract surgery. ARVO 2024 annual meeting. 5. Shabani H, De Ridder J, Asaad A, et al. Worldwide analysis of climate-related determinants of keratoconus. ARVO 2024 annual meeting. 6. Hwang B, Pecsok M, Cheng BT, Lambert SR. Rates of failure of corneal crosslinking for keratoconus in the United States. ARVO 2024 annual meeting. 7. Berntsen DA, Sinnott L, Orr DJ, et al. Axial growth after discontinuing soft multifocal contact lens wear in the Bifocal Lenses In Nearsighted Kids 2 (BLINK2) Study. ARVO 2024 annual meeting. 8. Wang T, Green N, Bi H, et al. The myopia control effect in children wearing orthokeratology lenses with different back optical zone diameters. ARVO 2024 annual meeting. 9. Huang JJ, Gorman B, Barr PB, et al. Multi-ancestry genome-wide association study of dry eye disease in the Million Veteran Program. ARVO 2024 annual meeting. 10. Chen A, Augello P, Asbell PA, Ying G. The repeatability of tests for dry eye signs in the Dry Eye Assessment and Management (DREAM) study. 11. Nagino K, Inomata T, Midorikawa-Inomata A, et al. Evaluation of maximum blink interval for the detection of dry eye cases with discrepancy between subjective symptoms and corneal findings. ARVO 2024 annual meeting. 12. White ER, Fazio N, Galenchik-Chan A, et al. Analysis of artificial tear effects on objective noninvasive dry eye parameters. ARVO 2024 annual meeting. 13. Pang Y, Parikh M, Sicks L. Lifestyle risk factor for dry eye symptoms in children aged 5 to <18 years. ARVO 2024 annual meeting. |


