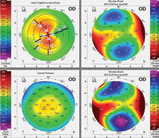
Irregular astigmatism occurs when the principle meridians are not 90 degrees apart and different parts of the same meridian have different degrees of curvature (Figure 1). Irregular astigmatism causes a reduction in the best-corrected spectacle acuity, a scissors reflex on retinoscopy and, most notably to patients, monocular diplopia, blurred vision and glare/halos.
Traditional treatment for irregular astigmatism has been rigid gas permeable (GP) lenses, which can provide superior vision compared with spectacles.1,2 While these lenses work well at masking corneal irregularities, they often require a significant adaptation period for patients. Sometimes, these lenses simply are not be the best option for some situations, such as outdoor activities or sports. The CLEK study showed that 27% of keratoconic GP wearers reported contact lens discomfort.3
When irregular astigmatism patients are unable to obtain adequate vision in glasses and are GP lens intolerant, alternative contact lens options are available, such as piggyback systems, hybrid and scleral lenses. While these options may be helpful by providing good vision and improved comfort, some patients find them inconvenient, their size intimidating or application and removal challenging. Soft contact lens designs can serve a place for these patients, allowing them to remain in contact lenses.
 |
| Fig. 1. Topography of irregular astigmatism secondary to radial keratometry. The blue areas indicate areas of flattening due to differing incision depths. Click image to enlarge. |
Standard Soft Lenses
Standard soft toric lenses have limited effectiveness for the irregular cornea patient. Their best application is in mild cases of irregularity where the topography is symmetrical centrally, there’s minimal optical distortion and adequate vision is achievable in glasses (Figure 2). Benefits of standard soft lenses outside of patient comfort and cost is that they’re readily available in most eye care practices. There are many replacement options, and most practitioners have expertise in fitting them. The downside to commercial soft lenses is that they don’t correct irregular astigmatism and may exhibit rotational instability with greater amounts of cornea irregularity. These lenses are a good option for patients who do not have critical vision needs and desire spectacle independence, despite seeing well with them.
Custom Soft Lenses
An increasing number of lathe-cut custom soft lenses are available for those with irregular astigmatism. This modality now encompasses more than 18 designs, some available in both hydrogel and silicone hydrogel materials. Custom soft lenses offer better initial comfort, centration and vision when standard lenses fail. They can be manufactured in virtually any parameter, including steep base curves and almost any conceivable sphere power, with cylinder and axis down to a single degree.
The downside for custom lenses is that some designs have multiple parameters to consider. Diagnostic, instead of empirical, fitting is necessary, and they’re made-to-order, which can take time for manufacturing. The lenses also are associated with higher cost, less frequent replacement, reduced oxygen transmissibility and comfort can be reduced compared with mass-produced standard soft lenses due to increased thickness. The ideal patients for custom lenses are those who have a decrease in best-corrected visual acuity with spectacles and traditional soft toric contact lens options with mild to moderate irregular astigmatism.
 |
| Fig. 2. Pentacam of mild keratoconus with symetrical astigmatism. Click image to enlarge. |
Candidates
Patients who could benefit from soft lenses for an irregular cornea include:
- Unilateral or asymmetric cones
- Initial keratoconus fits (straightforward on mild to moderate cones, easier insertion and removal than sclerals or hybrids)
- Post-penetrating keratoplasty surgery
- Pellucid marginal degeneration (PMD)
- Post-refractive surgery patients who cannot wear standard soft lenses
- Patients who have had intolerance to GP lenses (corneal or scleral)
- Patients who dislike or cannot be fit with piggyback lenses
Other candidates include irregular cornea patients whose anterior corneal higher-order aberrations (HOAs) are primarily offset by their internal or posterior corneal HOAs. Recent studies of HOAs in patients with keratoconus have revealed a problem where the residual irregular astigmatism derived from the posterior surface of the cornea causes deterioration of vision with GP lenses.4
Standard GPs (hybrids and sclerals included) cannot correct internal HOAs or HOAs induced by the posterior cornea, only corneal aberrations. If the corneal HOAs are corrected with a GP lens, the patient will complain of worse vision with the GP lens—even if it’s a scleral—compared with their spectacle correction because the higher internal HOAs will manifest themselves.
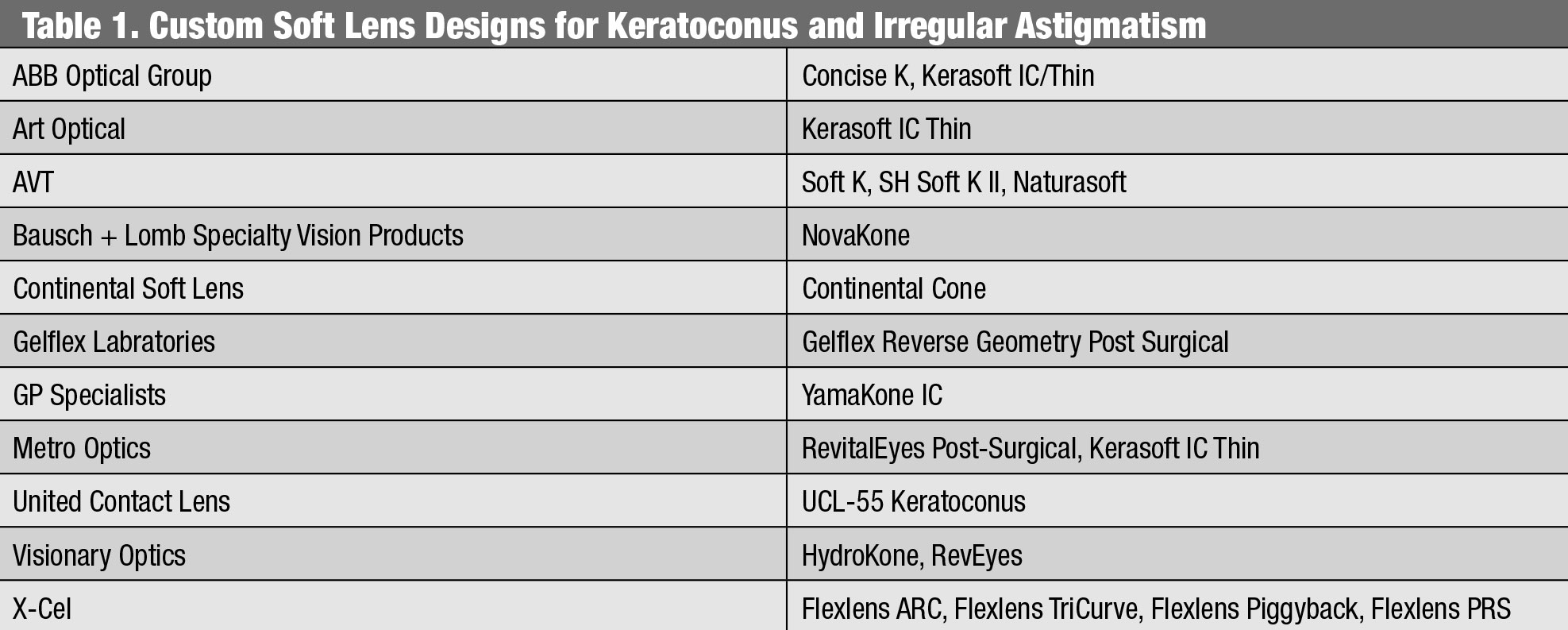 |
| Custom Soft Lens Designs for Keratoconus and Irregular Astigmatism. Click table to enlarge. |
Figure 3 displays a wavefront aberrometry measurement of a keratoconic eye. Looking at the point-spread function, the total HOAs (left) is much less than that of the corneal HOAs (middle image) and the internal HOAs (right). This patient is a poor candidate for any lens that will help correct the corneal HOAs with an increased center thickness. Doing so will cause the residual internal HOAs to become apparent. Instead, this patient is a great candidate for a thin custom soft lens that will drape well and employ aspheric optics. Future research into employing wavefront-guided correction technologies may offer a better clinical solution for managing residual HOAs for patients.5
Custom soft irregular cornea designs are unique from standard soft lenses since they have an increased center thickness (CT) to mask irregular astigmatism (Figure 4) or use an aspheric design to limit aberrations.
Many of these designs have a thickness of greater than 0.35mm to 0.40mm, so even with a latheable silicone hydrogel material, the resulting Dk/t does not meet the Holden-Mertz criteria of 24 x 10-9 units to avert hypoxia in daily wear.6
Outside of the optical zone, these lenses are usually lenticularized to reduce lens profile thickness, improving the overall comfort of the lens and increasing oxygen transmissibility over the corneal limbus. Clinically, they must move more (~1mm) than what clinicians are accustomed to seeing compared with standard soft lenses on normal cornea patients. The observed absence of corneal hypoxic findings in these wearers suggests that a significant amount of tear exchange occurs during lens wear. The use of silicone hydrogel materials can also help reduce the risk of corneal neovascularization.7 Still, there is a risk of neovascularization with this modality and these patients need to be monitored, especially if they have corneal incisions (post-RK and post-PK).
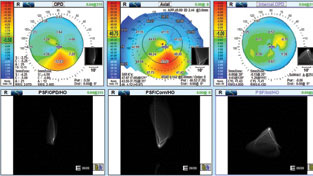 |
| Fig. 3. OPD3 wavefront aberrometry of a keratoconic patient. Click image to enlarge. |
Fitting Characteristics
Sagittal depth, or the height of the cornea, plays an important role in achieving a successful fit. Horizontal visual iris diameter (HVID), eccentricity, corneal curvature and scleral shape can impact it.8 Most designs are fit using diagnostic lenses by matching the sagittal height of the anterior eye with the sagittal depth of the custom soft lens. The corneal feature that has the greatest impact on sagittal height is the overall corneal diameter. For the same corneal curvature, the larger the cornea, the deeper the cornea will be. Sodium fluorescein (in the case of hydrogel materials) can help clinicians assess flat or steep fits during the diagnostic fitting process.
The base curve (BC) directly impacts vision, while the skirt or periphery directly impacts the fit. If the BC is too steep, it will reduce vision. Conversely, a BC that is too flat causes vision to fluctuate appreciably. Based on clinical experience, the appropriate BC will often be flatter than anticipated. The periphery can be altered separately than the central BC, which helps in achieving a fit absent of air bubbles as well as the necessary lens movement to facilitate tear exchange. If the fit appears tight and devoid of movement, then flatten the periphery. The converse is true when there’s excessive movement—steepen the skirt.
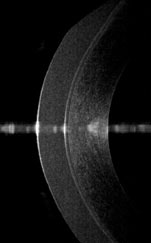 |
| Fig. 4. Specialty soft lens designs have a CT typically three to six times that of traditional hydrogel lenses. Photo: John Gelles, OD. Click image to enlarge. |
For lenses with a reverse geometry design, the reverse curve should be steepened or increased if there are bubbles in the midperiphery. If edge fluting is observed, then steepen the periphery or, in some cases, sectoral changes are required.
Some products offer a variety of thicknesses. A thicker lens will often improve the quality of vision by providing a smoothing effect over the central area of irregularity or ectasia. Use of a placido disc topographer during the fitting process will help determine the amount of thickness to employ depending on the amount of irregularity present in the mires on topography over the lens (Figure 5). Increasing the central thickness can also reduce halos and sometimes allow another line of visual improvement.
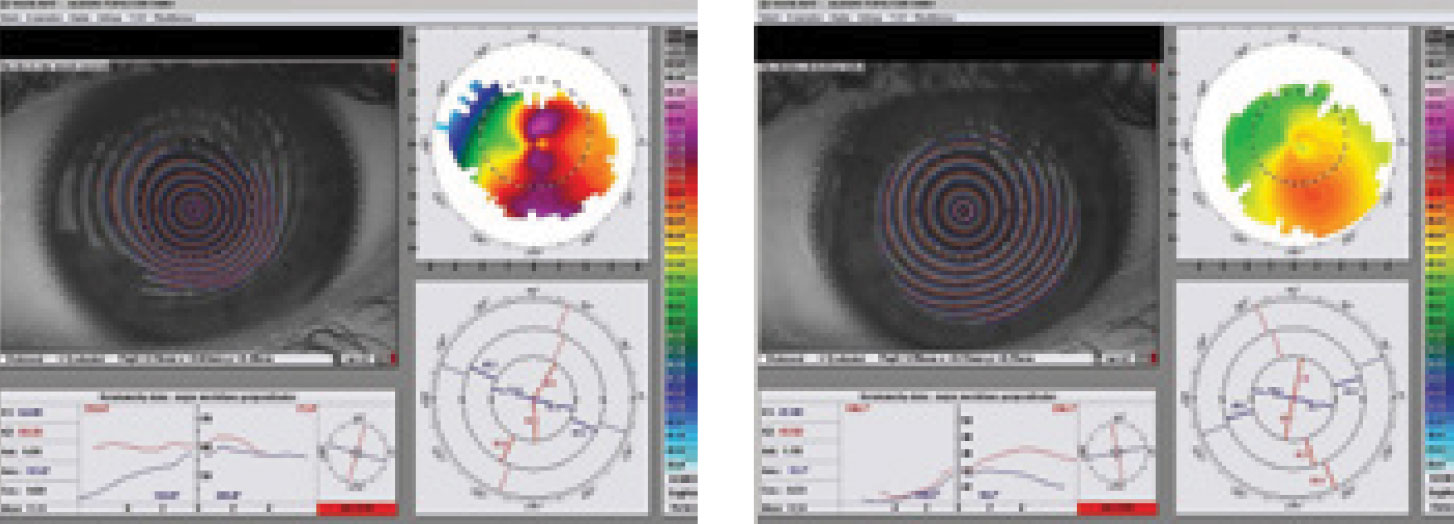 |
| Fig. 5. Topography of an irregular cornea can reveal the irregularity of the placido disc mires (left). Over-topography on the same irregular cornea with a custom soft contact lens with an increased center thickness of 0.65mm (right). Notice the mires are significantly more regular and the irregularity is “smoothed out.” Click image to enlarge. |
Where to Start?
In fitting custom lenses, perform a manifest refraction as well as a topography or Scheimpflug tomography of the anterior segment. Doing so will determine potential areas of concern such as a protruding graft or areas of corneal elevation. Evaluate anterior segment health to rule out preexisting staining, neovascularization or corneal microcystic edema. After gathering this basic data, determine the severity of the irregularity and corneal shape before choosing a lens design or diagnostic trial. Custom soft lens designs for the irregular cornea typically are more successful when there’s mild to moderate corneal irregularity allowing for a best corrected visual acuity equivalent to GP lenses, as opposed to more advanced irregularity and/or scarring.9,10
Lenses are fit with reference to the overall corneal shape rather than the steepest area on topography. To determine corneal shape, observe a side profile of the cornea. Have the patient look straight ahead in the slit lamp, rotating both the optics and the light source as close to 90º away as possible. Then use low magnification and a diffuser to evaluate the side profile of the cornea (Figure 6).
Looking at the corneal profile, ascertain whether the cornea is prolate or oblate (Figure 7). In an extremely prolate profile where there is a “ski-slope” like appearance to the cornea, a flatter skirt periphery may be required. In an oblate or “plateau-like” appearance, a reverse geometry design where the central BC is flatter compared with the secondary curve, may be necessary. If the corneal apex is within the central 4mm of the cornea, a standard geometry lens may achieve a better result; however, if the corneal apex is outside of the central 4mm, a reverse geometry lens may work better.
In addition, the practitioner should note whether there is a significantly decentered ectasia, which may indicate the need for a peripheral skirt adjustment or a sector design.
 |
| Fig. 6. Evaluate the corneal profile with a slit lamp. Click image to enlarge. |
Fitting Tips and Tricks
If the cornea is highly irregular, consider a design with variable or a reinforced center thickness. Bulking up the center of the lens may be necessary to enhance vision.
Once an initial lens has been selected and applied, evaluate the lens fit within five minutes using a dynamic assessment of movement, rotation, centration, comfort and vision. Allow the lenses to settle for 20 minutes before performing an over-refraction and assessing vision. Ultimately, if the over-refraction is unstable, then the central fit may not be optimal and indicate that a BC adjustment is needed.
If the patient’s visual acuity is clear immediately after a blink before slowly fading, the central fit is too steep—choose the next flatter BC in the fitting set. Conversely, if the patient’s vision is blurred after the blink and improves if they stare for a while, the central fit is too flat, and the next steeper BC is needed. A steeper peripheral skirt is indicated when there’s fluting and unstable rotation of the lens (Figure 8). Rotational stability is important, as high amounts of cylinder are often found upon over-refraction of these irregular corneas, and stability will allow for a good visual result.11
An automated over-refraction performed over the lens can help make sure enough cylinder is incorporated into the lens. The diameter of the lens should typically be 3mm bigger than the patient’s HVID to allow for appropriate draping.
 |
| Fig. 7. Observing the corneal profile can reveal whether it is prolate (left) or oblate (right). Click image to enlarge. |
Putting It All Together
Selecting a lens for managing irregular astigmatism includes many factors, and there are many options in the toolbox these days. Consider the severity of the irregularity, the location and size of the ectasia, the size of the cornea and eyelid fissures and the patient’s ability to manage the lens care and handling. Most patients who have been previously diagnosed with irregular astigmatism are aware they are challenging to fit with contact lenses, however, newly diagnosed patients need to be educated on their condition, the various contact lens options available to them and how complex contact lens management may be.
Managing patient expectations is always difficult but can be even more challenging when their vision is affected and cannot be corrected to the degree that the patient anticipates. Although specialty soft lenses have the advantage of quick adaptation, good comfort and being familiar to patients, they do not always correct vision as sharply as GP optics. Address visual expectations with the patient up front. If a patient is switching from a GP modality, they might lose a line or two of acuity. For patients who have irregular astigmatism and cannot wear another type of lens comfortably, this may be an acceptable compromise.
 |
| Fig. 8. Fluting will indicate if a steeper peripheral skirt is needed. Click image to enlarge. |
Despite some drawbacks, specialty soft lenses can be a great option for many irregular cornea patients, especially in improving patients’ quality of life.12 With the right pre-fit testing, patient selection and a firm understanding of the fitting process and challenges, specialty soft lenses can go a long way to improve patients’ vision and ocular comfort.
Dr. Andrzejewski works at Chicago Cornea Consultants with special areas of interest in the management of dry eye, keratoconus, and other cornea and contact lens-related issues, as well as scleral contact lenses. She also is an adjunct clinical faculty member of the Illinois College of Optometry.
1. Griffiths M, Zahner K, Collins M, et al. Masking of irregular corneal topography with contact lenses. CLAO J. 1998;24:76–81. 2. Jupiter DG, Katz HR. Management of irregular astigmatism with rigid gas permeable lenses. CLAO J. 2000;26(1):14-7. 3. Zadnik K, Barr JT, Edrington TB. Baseline findings in the Collaborative Longitudinal Evaluation of Keratconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39:2537-46. 4. Negishi K, Kumanomido T, Utsumi Y, Tsubota K. Effect of higher-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens. Am J Ophthalmol. 2007;144:924–9. 5. Marsack JD, Parker KE, Niu Y, et al. On-eye performance of custom wavefront-guided soft contact lenses in a habitual soft lens-wearing keratoconic patient. J Refract Surg. 2007;23(9):960-4. 6. Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthal Vis Sci. 1984;25:1161-7 7. Situ P, Simpson TL, Jones LW, Fonn D. Effects of silicone hydrogel contact lens wear on ocular surface sensitivity to tactile, pneumatic mechanical, and chemical stimulation. Invest Ophthalmol Vis Sci. 2010;51(12):6111-7. 8. Young G. Ocular sagittal height and soft contact lens fit. Cont Lens Anterior Eye. 1992;15(1):45-9. 9. Fernandez-Velazquez, F. J. Kerasoft IC compared to Rose-K in the management of corneal ectasias. Cont Lens Anterior Eye. 2012;35:175-9. 10. González-Méijome JM, Jorge J, de Almeida JB, Parafita MA. Soft contact lenses for keratoconus: case report. Eye Contact Lens. 2006;32(3):143-7. 11. Bennett ES, Barr JT, Szczotka-Flynn L. Keratoconus. In: Bennett ES, Henry VA, eds. Clinical Manual of Contact Lenses, 4th ed. Philadelphia: LWW; 2013:518-77. 12. Yildiz EH, Erdurmus M, Elibol ES, Acar B, et al. Contact lens impact on quality of life in keratoconus patients: rigid gas permeable versus soft silicone-hydrogel keratoconus lenses. Int J Ophthalmol. 2015;8(5):1074–7. |


