|
A 10-year-old Asian girl presented to the clinic for orthokeratology (ortho-K) to slow myopia. Her parents reported that her myopia was rapidly progressing. Both parents are high myopes— reportedly over -10.0D. Her entering visual acuity was 20/40-2 OD and 20/40 OS. Her most recent pair of glasses had a prescription of -6.75 -2.25x180 in the right eye and -6.00 -2.00x180 in the left eye.
Entry tests and slit lamp examination were unremarkable. Cycloplegic refraction was -7.50 -2.25x180 and -6.75 -2.00x180 with a best-corrected visual acuity of 20/20 OD and OS. Scheimpflug tomography (Pentacam AXL Wave, Oculus) showed Simulated Ks of 44.7D by 46.4D in the right and 45.1D by 47.0D in left eyes with flat axis of 001 and 179, respectively. Maximum keratometry was 46.8D OD and 47.2D OS; thinnest point was 503 and 490 OD and OS.
Using a multimetric analysis to identify irregular corneas (Belin/Ambrósio Enhanced Ectasia Display (BAD), Oculus) the final D value was 1.54 and 1.90 in the right and left eyes and axial length measurements were 26.18mm and 25.78mm, respectively. Horizontal white-to-white corneal diameter was 12.0mm.
Progressive axial length elongation (PALE) and keratoconus were discussed and treatment was initiated with soft toric center-distance multifocal lenses (Biofinity multifocal toric, CooperVision). On follow-up, the patient complained of poor vision and a laterally displaced position, with unstable rotation being observed.
The decision was made to move to a custom soft toric center-distance multifocal lens—the 54 Bifocal (SpecialEyes)—which was subsequently ordered. Visual acuity improved to 20/25 OU. The stability of vision improved, too, but the visual quality was still poor. To investigate this further, topography (E300, Medmont) over the soft lens was performed to determine the location of the optics, which were found to be bisecting the pupil.
Considerations
Here we highlight our thought process and consider how we would proceed:
Dr. Gelles: This is an interesting case with three issues.
- Obvious PALE.
- Poor optical centration of the contact lens.
- Potential keratoconus.
The corneal findings are very suspicious for keratoconus, with Kmax and the thinnest point falling right at the borderline. The BAD is the result of a multimetric analysis that analyzes anterior elevation, posterior elevation and pachymetry data, synthesizing the data into a single value representing the presence of an irregular cornea. A final D value less than 1.6 is considered normal, between 1.6 and 2.6 is considered suspicious and greater than 2.6 is considered abnormal. Again, here we are right on the borderline for the right eye and suspicious on the left.
As I stated previously in our June/July 2024 column, “Myopia Matters: How to Manage Progressive Axial Length Elongation,” the way I approach myopia control is similar to the way a surgeon approaches refractive surgery. If the cornea is normal and the prescription is within reasonable parameters, I will initiate a corneal-based treatment with ortho-K. If the cornea is suspicious, I will initiate a non-cornea based treatment with atropine, defocus soft lenses and/or spectacle lenses, which will preserve the anterior corneal metrics for comparison over time.
In this case, the cornea is suspicious and the refraction is high, thus ortho-K is eliminated as an option. FDA-approved defocus soft lenses to slow PALE (MiSight, CooperVision) are also out due to the high astigmatism. Biofinity’s center distance multifocal has a history of being used for myopia control in the BLINK study; it also has a toric option, so it was the natural initial choice for this case.1 However, the cornea is steeper and slightly wider in diameter than average, contributing to the unstable and off-centered fit.
The change to the custom toric center-distance multifocal soft lens provided much improved stability due to the customized parameters, but the lens was still slightly laterally displaced and the patient experienced poor visual quality. The choice to use a SpecialEyes lens was purposeful, as they have the ability to offset multifocal optics to shift them from the center of the lens to your patient’s visual axis (OptiSync Technology, SpecialEyes).
Dr. Su: This case presents some complexities. The patient already shows a high refractive error and an axial length >25mm. More notably, the corneal metrics seen on tomography suggest possible keratoconus, particularly in the left eye. Keratoconus is frequently overlooked in children and often isn’t screened adequately. Though this patient achieves 20/20 with correction, it’s crucial to recognize that in pediatric cases not correctable to 20/20, amblyopia might be diagnosed. However, amblyopia is a diagnosis of exclusion and should not be confirmed without evaluating corneal pathology through topography or tomography. It has been reported in the literature that children as young as four years old can have keratoconus, and this can be present with high cylinder and asymmetric astigmatism.2 Thus, corneal topography is essential.
As a practicing optometrist in Canada with access to myopia control spectacles, this is typically my first-line treatment as it can support corrections up to -10.00D sphere and -4.00D of cylinder. However, if the patient or parents find spectacles challenging due to resistance or an active lifestyle, soft toric lenses would be my next option. When this option is considered, though, it is always advised to have a backup pair of glasses. Ortho-K is contraindicated in this case due to the suspicion of keratoconus. Overnight wear of GP lenses that reshape the cornea could mask the signs of keratoconus, which could lead to a delayed diagnosis. In this case, a custom soft lens with adjustable decentered optics is a great option, as it offers enhanced stability and effective treatment zones not possible with standard soft lenses. Given the corneal conditions and PALE, I would monitor with biometry and topography every three months to track progression in corneal metrics and axial length changes.
Dr. Pfeifer: This can be a tricky case where the priority is to slow down any potential progression in such a young child, but her higher-than-average astigmatism and suspicion of corneal disease complicate the execution of myopia management. Soft toric multifocal contact lenses are often a great first choice of treatment for myopia management in those needing an astigmatic correction. However, decentration can often lead to intolerable reduced vision.
I like to confirm decentration is the cause by manually centering the lenses (using clean fingers) and asking the patient if things are suddenly clearer. Looking at alternative treatment methods, this patient would likely not appreciate clear enough vision in spherical multifocal contacts given her residual astigmatism. Also given the suspicion of keratoconus due to the elevated BAD values OU, I would avoid ortho-K for fear of increasing the likelihood of missing progression.
Avoiding the corneal astigmatism entirely, myopia control spectacles would be a great option; however, I am not yet able to prescribe them here in the US. Similarly, low-dose atropine remains an available option that could be considered. Another interesting option would be a center-distance multifocal bitoric corneal GP, as the refractive and corneal astigmatism match up very closely. This type of lens may improve visual quality for the patient and can be highly customized to deliver a great amount of peripheral myopic defocus. Some practitioners may find 10-years-old can be young to initiate daily corneal GP wear, but depending on the patient, they may be mature enough to take on some of that responsibility.
Regardless of what treatment modality is chosen, close monitoring of corneal tomography is important for any child for whom corneal disease is suspected. I would opt to monitor the child’s myopic progression with axial length measurements as well as monitor for any corneal changes with tomography every three to four months.
Discussion
This case highlights a few critical issues. First is to remember to look before you leap. A recent study sought to determine the prevalence of keratoconus in pediatric patients using Scheimpflug corneal tomography (Pentacam, Oculus). Out of 2,007 subjects aged three to 18, six were diagnosed with keratoconus, for a prevalence of 1:334.3 This finding suggests that keratoconus is more common in children than previously reported, highlighting the need for early and thorough screening during pediatric eye exams.
Patients are entitled to have more than one problem for us to tackle. We may know PALE is present, but keep keratoconus in the back of our minds as well. As these are both progressive, short interval follow-up every three to four months is prudent. In this case, if keratoconus does manifest, early intervention with crosslinking is necessary. Myopia is a sum of its parts, so ensuring corneal stability and directly measuring axial length is critical.
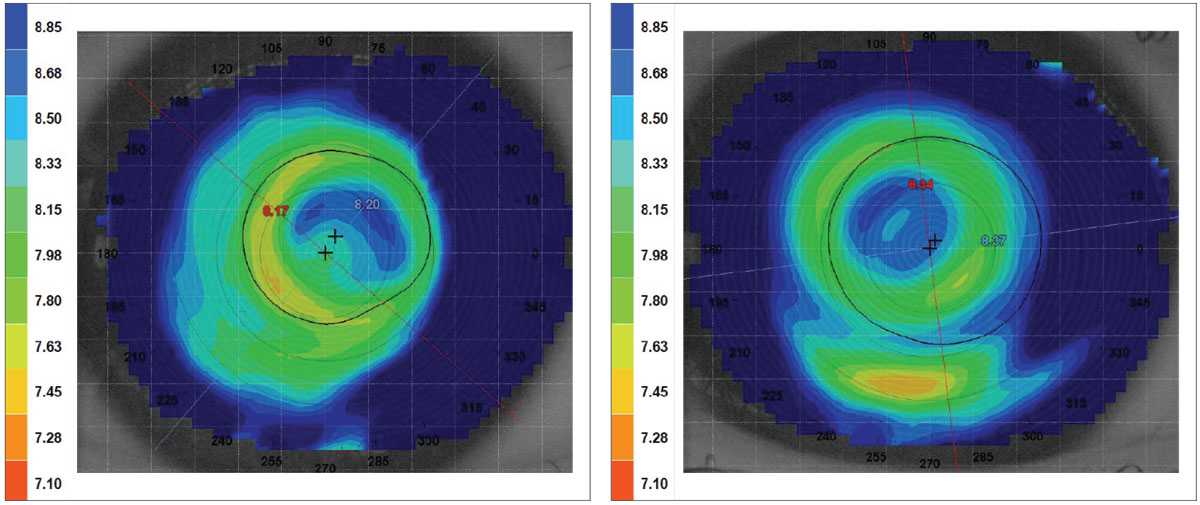
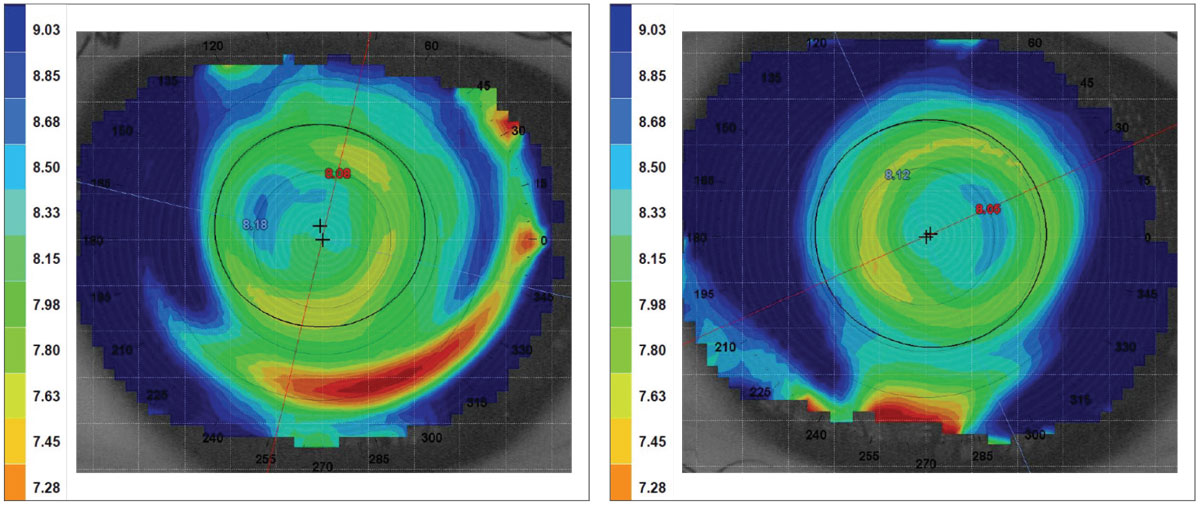
Poor visual outcomes can be attributed to lens instability or ill-aligned optics. Use of corneal topography over the lens can aid in locating the optical position. Use of the tangential map and a tight scale will allow precise viewing of position, and calipers available on most devices can measure the displacement to the line of sight, which can direct the decentration of optics to the line of sight.
Results
After topography over the lenses, the resulting tangential maps were used to measure the distance between the center of the multifocal optics and the line of sight. The displacement measured approximately 1.0mm and 0.9mm OD and OS, respectively. These measurements were given to the lab and OptiSync was used for the new set. At follow-up the patient reported improved visual acuity. On the tangential map, the shifting of the optics to the line of sight showed an improved optical position (Figures 1 and 2) and resulted in improvement in visual acuity to 20/20 OU.
 |
|
Fig. 1. Over topography of the patient’s right eye before (right) and after (left) moving the multifocal position. Click image to enlarge. |
 |
|
Fig. 2. Over topography of the patient’s left eye before (right) and after (left) moving the multifocal position. Click image to enlarge. |
After four-month follow-up, the patient’s cornea, axial length and refraction remained stable. The plan now is to follow her every four months to monitor for changes.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.
1. Walline JJ, Walker MK, Mutti DO, et al.; BLINK Study Group. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: The BLINK Randomized Clinical Trial. JAMA. 2020 Aug;324(6):571-80. 2. Mukhtar S, Ambati BK. Pediatric keratoconus: a review of the literature. Int Ophthalmol. 2018;38(5):2257-66. 3. Harthan JS, Gelles JD, Block SS, et al. Prevalence of keratoconus based on Scheimpflug corneal tomography metrics in a pediatric population from a Chicago-based school age vision clinic. Eye Contact Lens. 2024;50(3):121-5. |