|
Hybrid lenses have a unique contact lens design that is made up of a gas permeable (GP) center with a soft contact lens “skirt” attached. Many of us who fit hybrid lenses have run into the problem of lens adherence, sometimes so severe that patients cannot remove the lens. Lens adherence, although it generally does not go unmentioned by the patient, can cause corneal staining, conjunctival injection, rebound conjunctival hyperemia after removal and, in the late stages if not addressed, corneal scarring and neovascularization.
Adherence is typically caused by three things: (1) a lens that is applied too forcefully, (2) a lens with a GP portion that is too steep or (3) a lens with a soft skirt that is too steep (though this is much less common). As an example, when the base curve (BC) of a GP is too steep, the lens no longer aligns with the central cornea and its weight distribution shifts toward the edge. Mitigating this is as simple as flattening the BC.
Adherence can be simple to troubleshoot if you know what to look for during the exam and teach your patients proper lens application and removal. Here’s where to start.
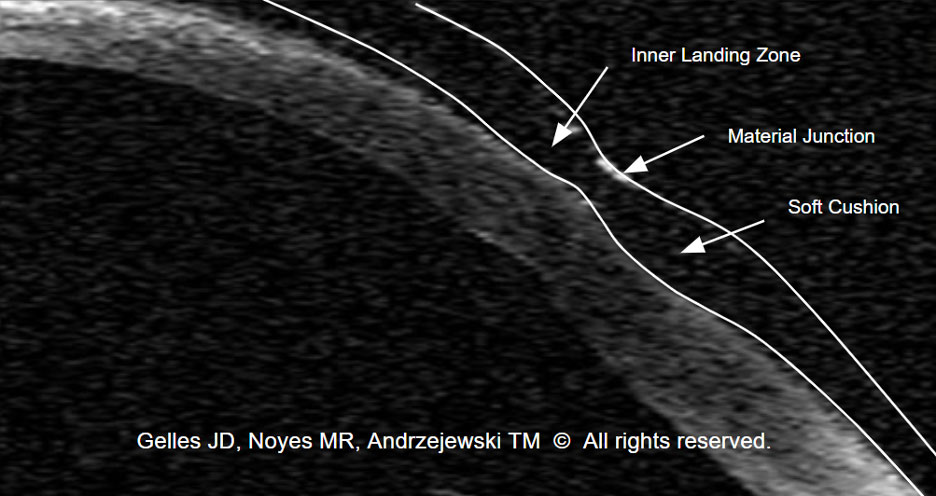 |
| Fig. 1. OCT of an ideal hybrid fitting relationship to avoid lens adherence. Click image to enlarge. |
Background
There are two main types of hybrids: those for normal corneas and those for irregular ones. Troubleshooting looks different for the two designs in regard to flattening the GP portion of the lens. With the normal cornea design, the goal—similar to corneal GPs—is to align with the cornea. The irregular cornea design is intended to vault the cornea with the goal of clearing it by approximately 100μm to 150μm at the time of the initial fitting and ~50μm within several hours of wear.
The weight of the lens is shared between the GP on the midperipheral cornea and the skirt, with 70% to 80% of support in the soft skirt and 20% to 30% in the inner landing zone of the GP portion (Figure 1). If the balance varies too much, then lens adherence can result (Figure 2).
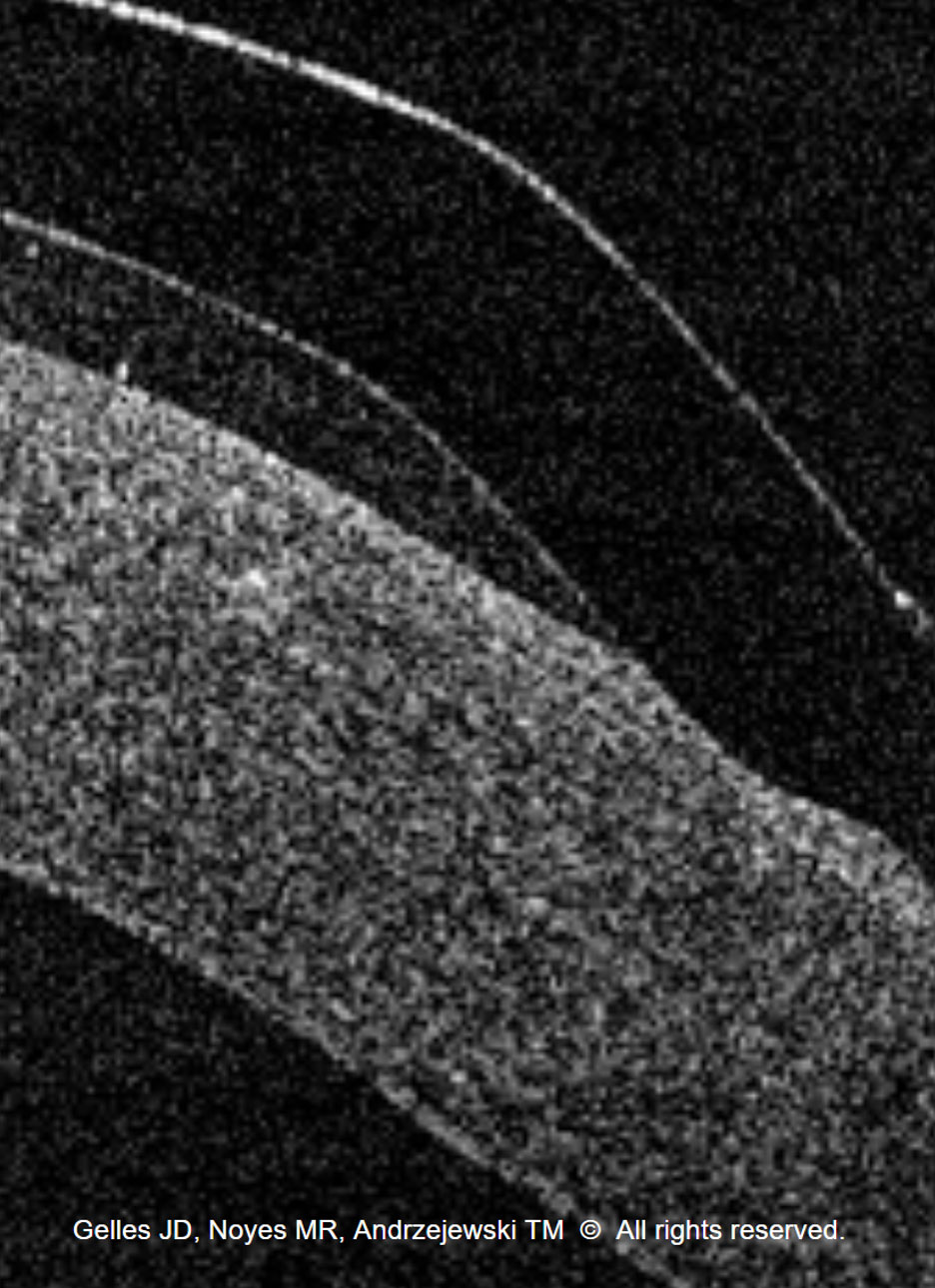 |
| Fig. 2. OCT of a hybrid with inner landing zone bearing leading to lens adherence, as the support of the lens is more toward the edge of the GP vs. the skirt. Click image to enlarge. |
Assessment
There are several ways to identify lens adherence, the first being patient history. Patients experiencing issues will report difficulty removing the lens at the end of the day or increasing discomfort with longer wear times.
The second is slit lamp exam. With lens wear, there will be no movement and potential inferior displacement. Evaluation upon removal will typically show evidence of epithelial disruption on the cornea in the junction where the GP and the soft skirt meet (Figure 3).
As the tear exchange is much slower with hybrids than corneal GPs, it doesn’t make sense to apply fluorescein over the lens. However, it’s imperative that the lens is removed and fluorescein is instilled afterward to monitor for any staining.
Central staining is always an issue of the BC being too flat or the sagittal depth/vault being too low. Midperipheral staining, on the other hand, can be either a BC, sagittal depth or skirt issue. To determine where the problem lies, the lens should be reapplied with fluorescein in the bowl to check the pattern with gentle application by the practitioner to rule out whether the patient applied the lens too forcefully.
The fluorescein pattern should exhibit central clearance in the GP portion of the lens, a light halo of thinning at the inner landing zone (the border between the GP edge and the soft skirt) and bearing in the skirt outside the GP junction. Reapplying a diagnostic lens with 100μm less vault can confirm there is not excessive vault if heavy central bearing is present; if clearance is present, no matter how thin it is, then the patient’s lens has too much sagittal depth.
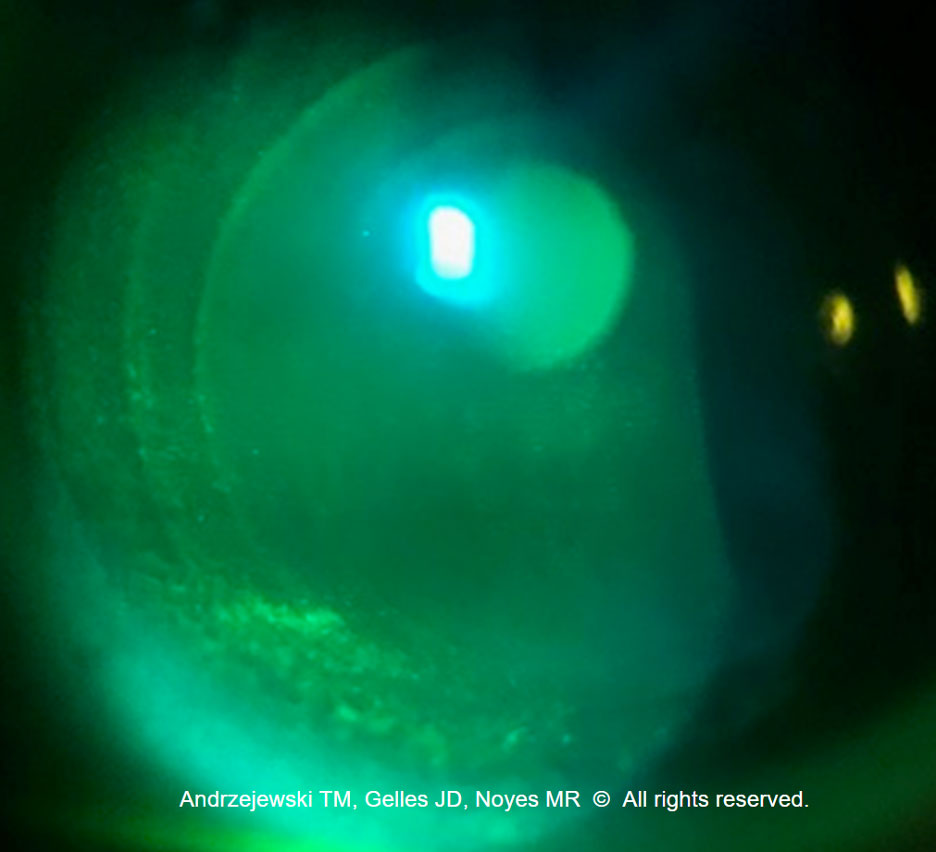 |
| Fig. 3. Midperipheral corneal staining, indicated by the seal-off around the GP edge of the hybrid. Click image to enlarge. |
Problem-Solving
For the normal cornea design, clearance can be solved by flattening the BC by at least 0.1mm. For the irregular cornea design, if there’s central clearance, decrease the vault 100μm until bearing is observed. If there’s light bearing, add 50μm to the final lens upon ordering, but if there’s heavy bearing, add 100μm.
After the vault is confirmed to be acceptable, the next option is to steepen the skirt if bearing in the inner landing zone still remains. Be careful to not fit the skirt too steep because the second-generation irregular cornea design has a silicone hydrogel skirt, which temporarily lifts the GP junction off the cornea before the lens settles and allows the edge of the GP to dig into the cornea after it has been on the eye for a couple of hours (Figure 4).
In some cases, a hybrid lens may not be the right choice. The cornea may have a markedly displaced apex inferiorly, be too irregular or have too much eccentricity to accommodate the lens shape, in which case alternative lens designs exist for you to achieve success.
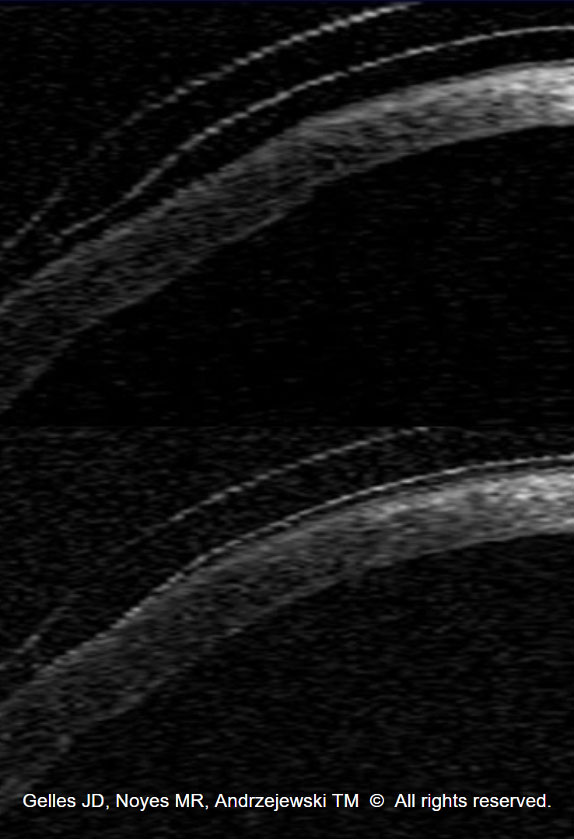 |
| Fig. 4. OCT of the lens on the eye with a skirt that’s too steep at dispense (top). OCT post-dispense shows the lens has settled too much and now bears into the cornea (bottom). Click image to enlarge. |
Takeaways
Hybrid lenses have a unique design that can allow for fitting advantages, specifically when it comes to irregular corneas. Technology such as OCT imaging can aid with particularly troublesome fits, but much of the troubleshooting is observable simply by slit lamp observation and fluorescein dye. Lastly, ensuring proper patient adherence and insertion/removal techniques is paramount for a successful fit. Commit these fit tips to memory and you’ll be well on your way toward becoming an expert specialty lens practitioner, hybrid lenses included.
Dr. Andrzejewski practices at Chicago Cornea Consultants and serves as an adjunct assistant professor of optometry at the Illinois College Optometry as well as the Chicago College of Optometry. Her clinical work is dedicated exclusively to specialty contact lenses and surgical comanagement. She is associated with Bausch + Lomb Specialty Vision Products, Blanchard, Eaglet, Ocular Therapeutix and SynergEyes.