 |
When I started as a contact lens specialist, the best advice I received was to understand and perfect a lens in each category. After gaining more experience, I realized having several lenses in your repertoire has its advantages. While I have a few go-to lens designs that I use most of the time, I am also able to defer to other options. In the following case, I ended up choosing a scleral lens design that I don’t use as often but was well suited for my patient.
The Case
A 21-year-old female presented with complaints of blurred and fluctuating vision that was giving her headaches and making it difficult to concentrate in school. She was using reading glasses on top of her contact lenses. She had tried a handful of different lenses, including rigid gas permeable (RGP) lenses that she could not tolerate and hybrid lenses that gave her the most consistent and clear vision but were very dry, and finally settled on Cooper Biofinity toric lenses that gave her good comfort but fluctuating and unclear vision.
A month ago, she was screened by a pediatric ophthalmologist to rule out accommodative disorders and strabismus. The exam findings were unremarkable, and she was cleared.
Her contact lens prescription was +5.25 -0.75x170 OD and +5.50-0.75x180 OS. Her presenting visual acuities (VAs) were 20/30+ OD and 20/25- OS. Over-refraction yielded -0.50 20/25+ OD and plano OS.
The patient’s cover test revealed ortho at distance and at near. Her accommodative amplitudes were to the nose OU. Her positive and negative relative accommodations were within normal limits. Her pupils were round, equal and reactive to light. Her confrontation fields were full-to-finger counting.
Topographical imaging revealed irregular asymmetric bowties OU with simulated keratometry readings of 43.32@092/40.86@002 OD and 42.94@086/ 40.52@176 OS and horizontal visible iris diameters (HVIDs) of 12.0mm OU (Figure 1).
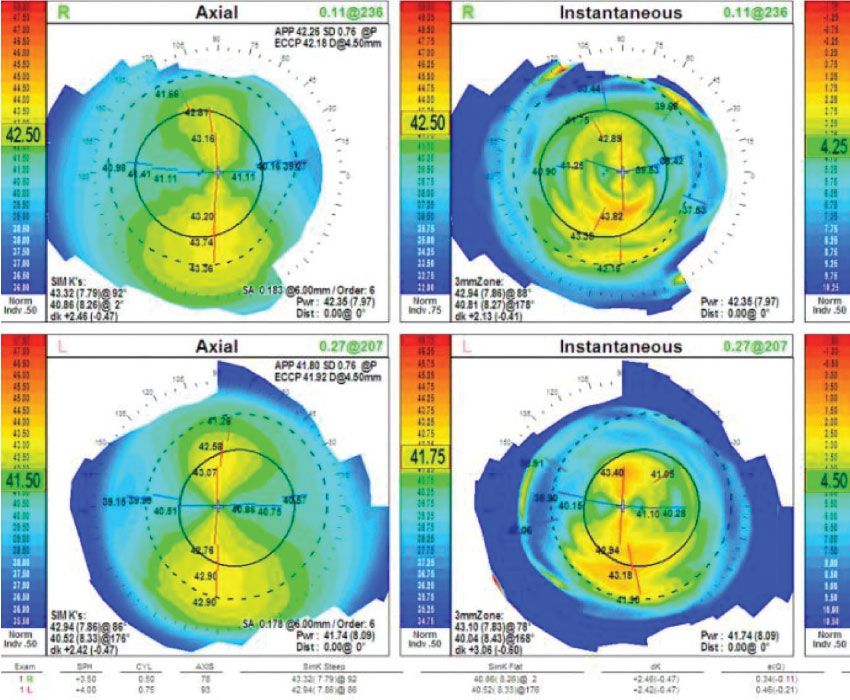 |
| Fig. 1. Topography showed asymmetrical bowties and slightly irregular astigmatism OU. Click image to enlarge. |
Her slit lamp exam revealed clear lids and lashes and clear conjunctiva with deep and quiet anterior chambers OU. Her corneas, irises and lenses were normal. Her intraocular pressures were 15mm Hg OD and 14mm Hg OS.
Contact Lens Evaluation
Manifest refraction revealed:
+4.00+1.00x078 (VA of 20/25+) OD
+4.25+1.00x087 (VA of 20/30) OS
After reviewing the patient’s results, I discussed contact lens options with her. Given her previous success with hybrid lenses and her dryness issues and irregular astigmatism, we decided on scleral RGP lenses. I placed diagnostic lenses with a base curve (BC) of 8.04/-2.00/sag 4.6 and a diameter of 16.9mm on both eyes.
Both of her eyes exhibited an excessive sagittal clearance of 400 and dropped low. The chamber size was small for the HVIDs even after pushing the lenses up. Over-refraction yielded +5.25 OD and +5.00 OS and brought the patient’s VAs to 20/20- OU. The patient was thrilled with the comfort and vision these lenses provided, so we decided to move forward with them.
The BC of the lenses was flattened to address the increase in vault from increasing the diameter to accommodate the patient’s larger-than-normal HVIDs. Changing the BC increased the power of the lens. The sag was also lowered to achieve a vault of 200μm. I ordered scleral lenses from Advanced Vision Technology with a BC of 9.08 OU, a diameter of 17.1mm OU and powers of +9.50 OD and +10.00 OS.
After the diagnostic contact lens fitting, I dilated the patient with Cyclogyl to complete her exam. The cycloplegic exam revealed +4.50+1.25x085 OD and +4.75+1.25x087 OS with VAs of 20/25+ OD and 20/30 OS.
Cycloplegic refraction did not show a significant amount of latent hyperopia compared with the dry manifest refraction. The dilated view of the posterior segment revealed a cup-to-disc ratio of 0.25 OU. Everything else was within normal limits. I concluded that the patient had hyperopia with irregular astigmatism OU.
Original Dispensing
The patient returned for a dispensing visit the following week. I placed the lenses and evaluated the lens fit and her vision. Her VAs were 20/40- OD and 20/60 OS. The central vault was 200μm OU, but the lenses were dropping low. When the lenses were pushed up, the patient’s vision improved. Autorefraction showed an optic that was decentered inferiorly (Figure 2). I did not perform over-refraction due to the decentered lens optics.
 |
| Fig. 2. Autorefraction of the lens over the eye exhibited inferiorly decentered optics. Click image to enlarge. |
I ordered scleral lenses with the original BC, diameter and powers in addition to a 2D toric haptic OU to raise them up and a thinner center thickness to reduce their weight.
Dispensing Redo
The lenses were placed on the patient’s eyes a week later. They exhibited some improvement in centration but were still decentered. Her VAs were 20/30- OD and 20/40- OS.
After returning to school, the patient would not be able to come back for follow-up visits, so I decided to refit her in a different design to see if I could achieve a better fit.
I chose the Europa lens from Visionary Optics with a 16.0mm diameter to reduce the mass of the lens and achieve a lighter center of gravity and BCs of 40.00 OD and 42.00 OS. The central vault of the right lens was 200μm with good limbal clearance, and the central fit of the left lens was slightly excessive at about 300μm. Over-refraction brought the patient’s vision to 20/20- OU. Even though this lens diameter was smaller than the previous, the limbal vault was slightly excessive. The following lenses were ordered: 40/+5.50/15.7 standard periphery BXO clear OD and 41/+4.50/15.7 standard periphery BXO blue OS.
Since we did not need to adjust the sag or diameter much, the power of these lenses was roughly half of the original scleral lens order. I anticipated that this would produce good centration and a better fit.
Dispensing Take Three
The patient returned a week later, and the Europa lenses were placed on her eyes. Her VAs were 20/25+ OD and 20/25- OS. An over-refraction of +0.50 OU brought the patient’s vision to 20/20- OU. The central vault of 200μm and the limbal vault were adequate OU. The patient was thrilled with the vision and comfort the lenses offered, so I ordered them.
Follow-up
The patient returned a month later and had no complaints. For the first time in years, her vision was consistently clear, she no longer needed reading glasses and her eyes were comfortable. Her prescription was finalized.
Discussion
In this modern age of scleral lenses, we have many designs to choose from. Some don’t use BC to dictate sagittal height, which is advantageous for high minus keratoconus patients. For example, some sclerals have a standard flat BC that doesn’t change with changes in sagittal height.1 Instead, BC is used to address limbal fit in these lenses. A -23.00D keratoconus patient wearing RGP lenses may be a -8.00D in a scleral lens because of the difference in BC when it is not dependent on the curvature of the cornea. Lower powers can improve optics, lens mass and patient comfort. However, if a patient is already a high plus, transitioning between designs like this can be disadvantageous and cause lens decentration in a scleral lens, which results in induced astigmatism and poor vision.
Choosing a design that is closest to what the patient needs on diagnostic fitting is something I learned how to do quickly to reduce chair time and increase patient satisfaction. HVID, diagnosis, scleral shape, material availability and refractive error are all factors that need to be assessed immediately for the best lens fit and lasting patient success.2
|
1. Hellem A. SynergEyes. A lens designed to fit true scleral shape. blog.synergeyes.com/blog/a-lens-designed-to-fit-true-scleral-shape. Accessed March 27, 2019. 2. Johns LK, Barnett M. Contemporary scleral lenses: theory and application. Bentham Science. 2017. |


