 |
There has been a lot of talk lately about how to build a specialty lens practice, as practitioners look to maximize their revenue and establish a niche. Fitting specialty lenses can be endlessly rewarding, with patients returning year after year because your talents help them live their best lives. So, what can you do to build GP and specialty lens fitting in your practice and, ultimately, change more lives this year?
Fitting Sets
The first step is to ensure you have the tools necessary to fit any patient who enters your practice. While spherical GP lenses are often ordered empirically these days, many specialty lenses still require a fitting set and diagnostic fitting process. Even our most advanced scleral profilometry technologies still work best in concert with a diagnostic fitting in office to determine the initial lens power. That’s not to say you need every single fitting set under the sun; many laboratories will lend you a fitting set for a prescribed amount of time if you wish to fit a particular patient.
 |
|
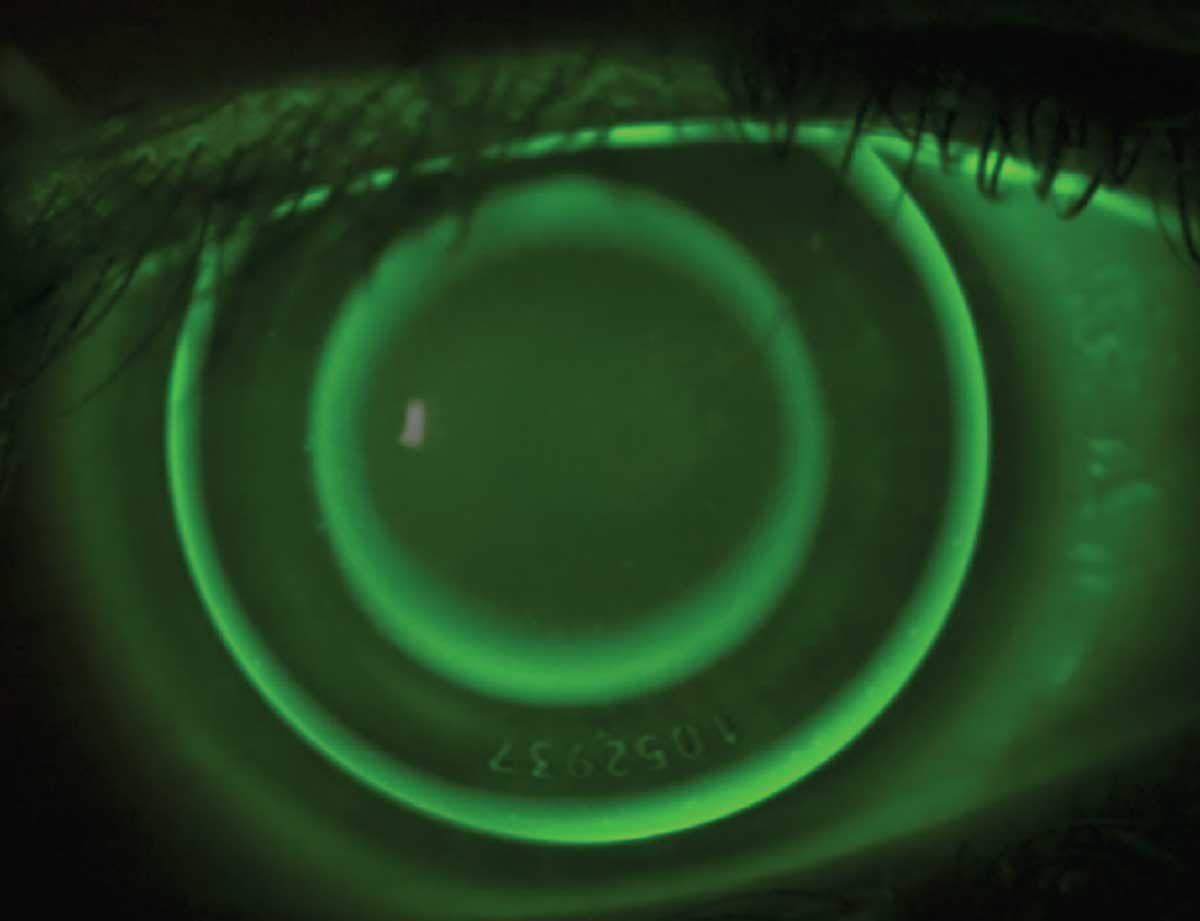
Fig. 1. A well-centered, empirically designed orthokeratology lens is evaluated on-eye at the dispensing visit. The sodium fluorescein dye is absent in the central treatment zone and midperipheral alignment curves. Click image to enlarge. |
In general, the lens fitting sets I would consider essential include: a corneal keratoconic GP set, a corneal reverse geometry GP set, a scleral GP set (preferably with two different diameters and toric haptic options) and an irregular cornea hybrid lens fitting set. If you wish to order spherical GP, bitoric GP, regular cornea hybrid or orthokeratology (ortho-K) lenses, there is a very high success rate with empirical fitting; thus a lens fitting set is optional. I find the same is true for simultaneous GP multifocal lens designs.
There are empirical lens fitting options available for irregular cornea hybrids, but I highly recommend getting in touch with the laboratory’s consultation team prior to attempting such a fit so you can obtain all necessary data at the patient’s initial fitting visit.
 |
| Fig. 1. A well-centered, empirically designed orthokeratology lens is evaluated on-eye at the dispensing visit. The sodium fluorescein dye is absent in the central treatment zone and midperipheral alignment curves. Click image to enlarge. |
It is useful to have a fitting set for a translating GP multifocal design, as you can determine in-office how the initial lens fits and where the segment height is relative to the pupil center. However, the final power of the lens affects the overall weight, therefore impacting the final placement of the segment height, the diameter and the amount of prism needed for optimal lens movement and stability.1 Some fitting sets will have varying lens powers to assist with this unique scenario.
Patient Referrals
The next step is to ensure you have patients to fit. Network with local practitioners to let them know you have a passion for GP lenses. You may be able to grow your ortho-K practice by meeting with local pediatricians or primary care providers, and you may also find success in growing your scleral lens practice by offering your services to both corneal specialists and general ophthalmologists.
Once these specialty fits are complete, follow-up with the referring practitioner to thank them for their referral and share the results of your fitting success. This, along with word-of-mouth referrals from happy patients, can result in more patients entering your practice.
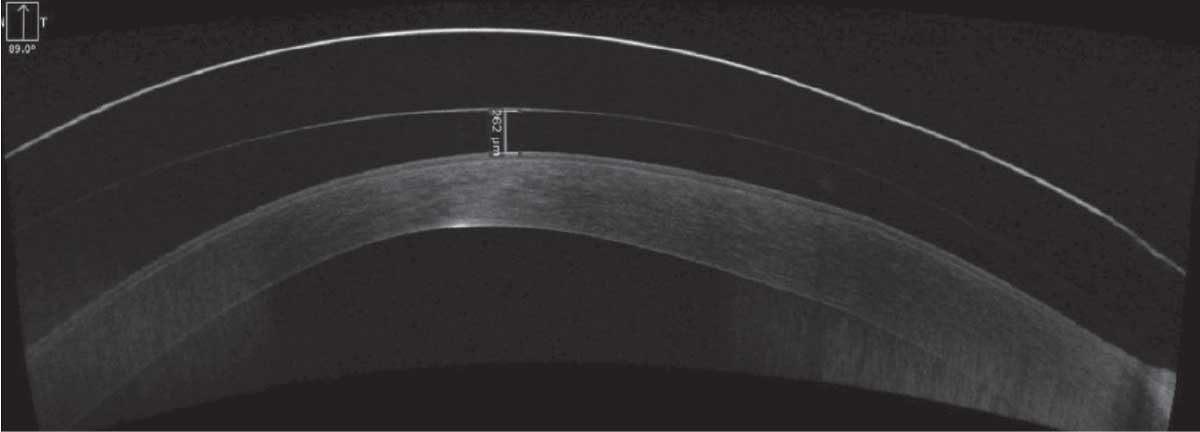 |
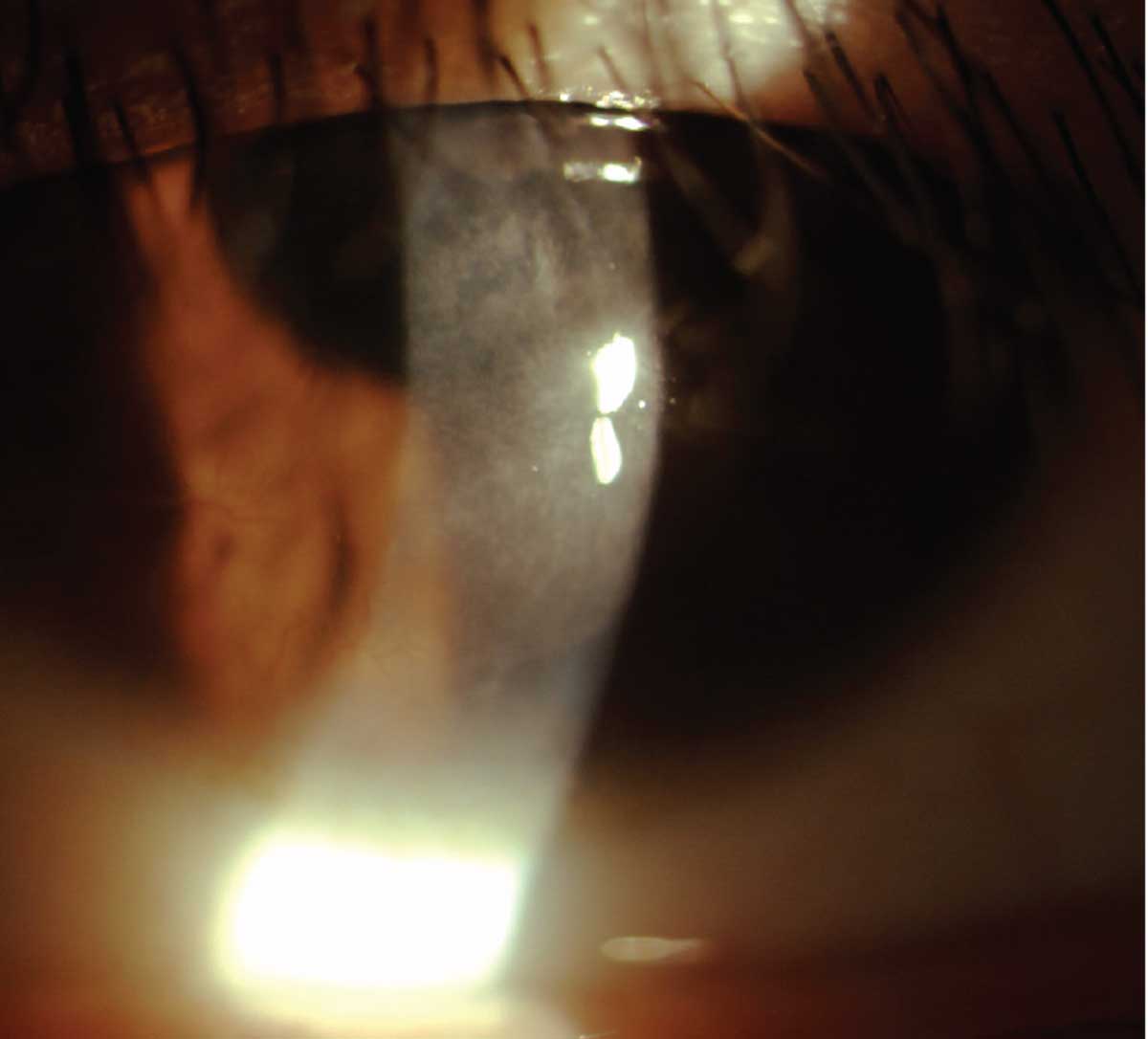
| Fig. 3. This scleral fit was decentering inferiorly, as shown on an anterior segment OCT (the tear film reservoir depth is greater inferiorly, seen on the left side of the image). The decentration was resolved by reducing the central vault and steepening the scleral landing zone. Click image to enlarge. |
Diagnostic Equipment
It can be useful to invest in specialized diagnostic equipment to fit these lenses, though this is not always required (nor are you required to have the fanciest version of every item listed). For ortho-K, it is essential to have a corneal topographer because it tells you so much more about how the lens fits on the eye, at night, when the eye is closed. These findings don’t always translate to what we see in the manifest refraction, over-refraction or a sodium fluorescein pattern assessment on the open eye.
If you are fitting specialty lenses on irregular corneas, it may be worth investing in corneal tomography so that you can image the posterior corneal surface and have global pachymetry readings. If you intend to have a heavy scleral lens practice, profilometry and anterior segment optical coherence tomography are worthwhile considerations. There are instruments which combine several of these imaging options so you can ensure your investment will meet any current and future needs.
 |
| Fig. 4. Patient with scleral prolapse, which was resolved with the assistance of a laboratory consultant. This image was uploaded to the lab’s web consultation tool, along with other fitting data, and they replied via email with suggested changes to the fit, which included reducing the lens diameter. Click image to enlarge. |
An imaging system may also be useful as you communicate your findings to GP lab consultants. I cannot tell you the number of emails I send to consultants (my apologies to all the lovely consultants out there I work with) with my written findings, but then I also say “see attached image” to help better communicate what my words may fail to convey. My photography and anterior segment OCT skills don’t always communicate everything flawlessly, but there have been times that a consultant’s assessment of an included image has helped optimize my lens fit for the better.
With all that said, there are also times when it’s easier to communicate these findings and challenges via phone; it may also be worth following up your email with a phone call in tough cases.
Passion and Persistence
Yes, these are qualities you can possess and not tangible tools to purchase and implement; however, passion and persistence are essential to your success when building a practice around GP and other specialty lenses. Your passion for these patients will carry you through even the toughest cases you encounter. Your persistence will give you the ability to succeed when the going gets tough. So, get going!
1. Truform Optics LlevationsThin (Multifocal) Contact Lens Fitting Guide. www.tfoptics.com/presbyopic/documents/llevationsthinfittingguide.pdf. Accessed January 25, 2021.


