 |
A recent patient visit reminded us of the myriad reasons we recommend annual eye examinations for contact lens wearers. A 53-year-old keratoconus patient wearing corneal gas permeable (GP) lenses had been wearing the same pair for the last decade with no interim examinations.
The present visit opened up a much-needed dialogue, and we were able to mutually agree that changes to her routine and lenses were necessary. In the decade since her last visit, advancements in contact lens designs and care have allowed us to better meet her needs.
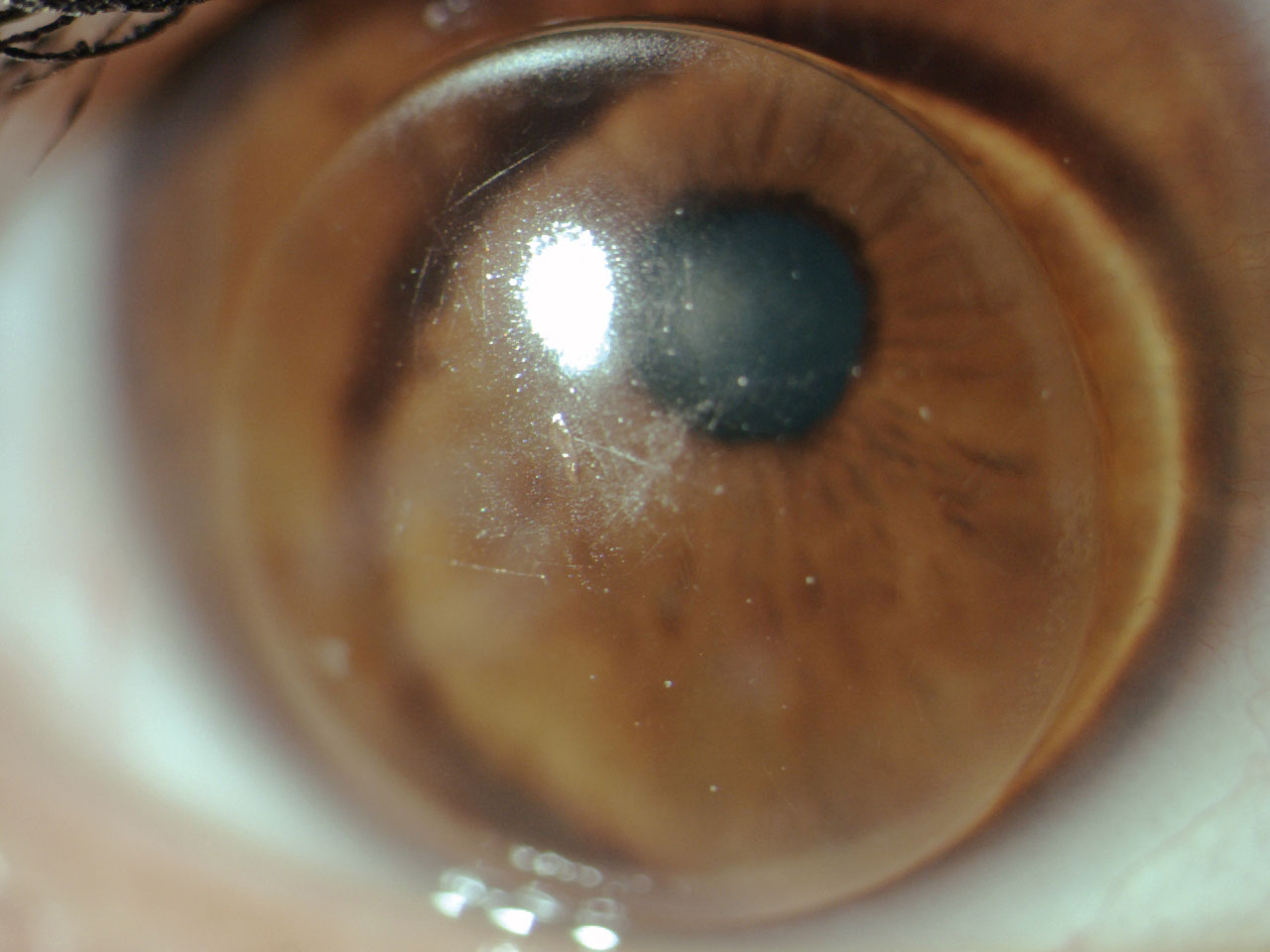 |
| Fig. 1. GP lens with central scratches, deposits and makeup debris at the edges. Click image to enlarge. |
Ask the Right Questions
Given that a good case history is key to any patient visit, asking the right questions to uncover unspoken issues that contact lens wearers have will get us beyond “everything is fine” and to the real story.
This patient initially relayed that everything was great with her lenses, including her vision. She didn’t feel she was having any problems other than a single emergency room visit for a red, irritated eye, where she received unknown eye drops for treatment. She said that issue cleared up shortly after the visit and has not recurred.
We asked her to elaborate on how she uses her eyes at home and work and about any specific potential symptoms she may have encountered. The patient then admitted to repeated episodes of eye irritation over the last few years. She also confirmed persistent daily dryness that had been worsening over the past few months as she struggled with working from home and increasing use of digital devices. She then admitted to having difficulty seeing up close with her lenses, which had been worsening over time. Also, she described a “greasy film” that had appeared in her vision over the past couple months. She then admitted noncompliance with the use of her current GP multipurpose solution and only occasionally rubbed her lenses in the morning before application.
We performed a slit lamp examination, which uncovered the underlying cause of this patient’s episodes of eye irritation. Her habitual lenses had numerous front surface scratches and deposits. The lenses were caked with debris at the edges (Figure 1). Her cornea had nasal and temporal (3 o’clock and 9 o’clock) staining. There was also peripheral corneal neovascularization with mild opacification consistent with previous episodes of vascularized limbal keratitis (VLK) present on each cornea (Figure 2).1
Her conjunctiva had a moderate papillary response with mild injection on the upper and lower lids. She also wore heavy makeup and presented with mascara, eyeliner and powder on each eyelid. She was not always compliant with nightly removal of her makeup.
We were able to perform a targeted dry eye workup, uncover the underlying causes of her dry eye and treat accordingly. We reviewed the importance of removing her GP lenses for cleaning nightly as well as complete removal of eye makeup nightly.
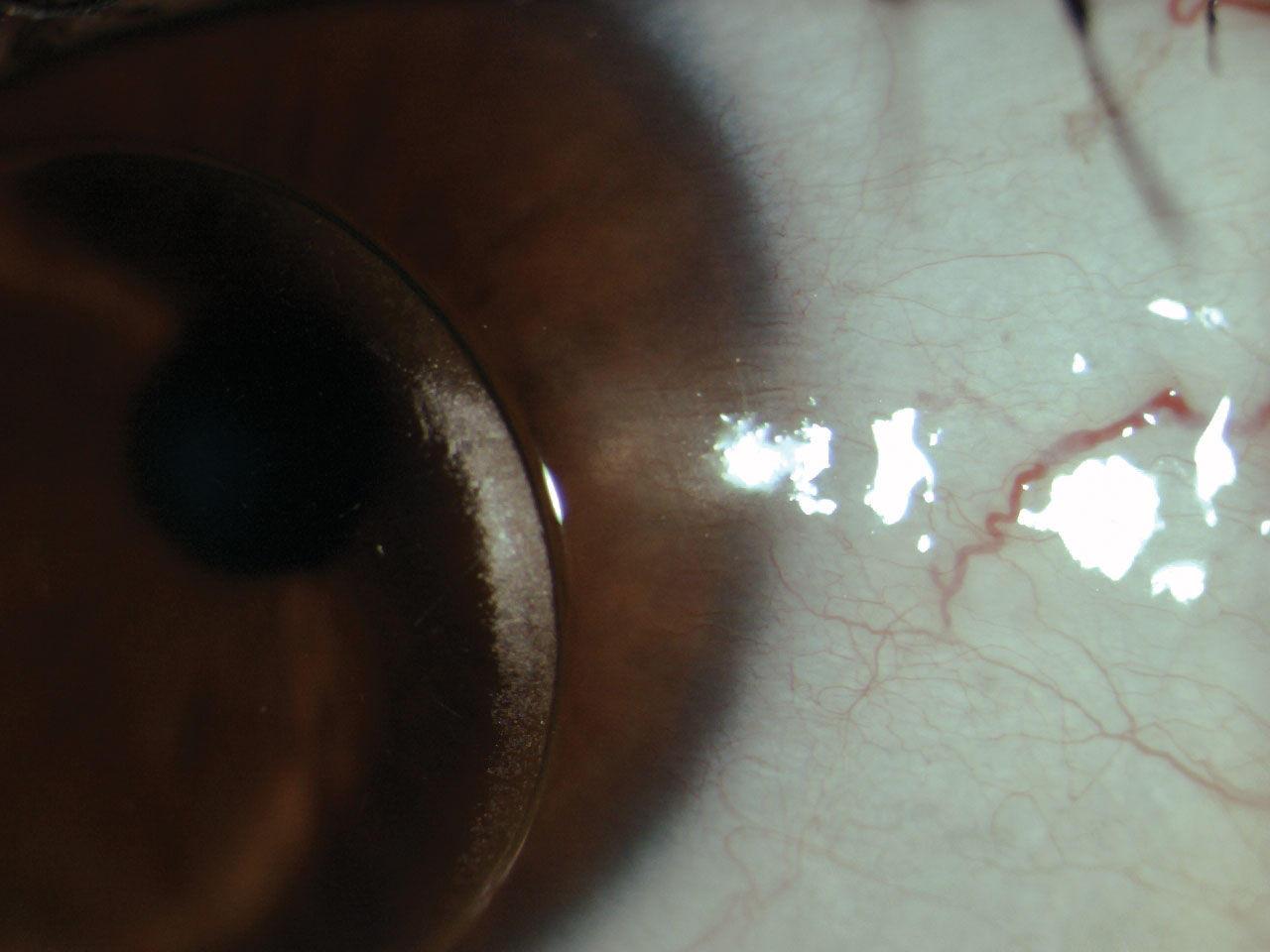 |
| Fig. 2. Scarring and neovascularization in the limbal region from VLK is visible. Click image to enlarge. |
Prevent Complications
Each time we see a patient, we gain an opportunity to review critical parts of lens wear and care. Since this patient hadn’t been to our office in a decade, she developed some bad habits that we felt could stand correcting. Given the age of her habitual lens, it was in definite need of replacement. Contact lens deposits can occur secondary to protein or lipid buildup and begin to occur within minutes of lens wear.2
Proper lens cleaning, including a rubbing step, is vital to reducing the bacterial bioburden on a contact lens. This patient was using Boston Simplus (Bausch + Lomb) solution, so we reviewed the best practices, including using fresh solution each night, soaking overnight (or at least for four hours) and rinsing for approximately five seconds with a steady stream of solution before lens application.3
We also reviewed proper handwashing and case cleaning protocols (discard used solution, rub and rinse lenses with fresh solution, wipe with a tissue, let air dry facedown and avoid using tap water).4
Contact lenses may come into contact with cosmetics during the application and removal process or when makeup is applied while lenses are on. Additionally, research has shown that cosmetics are released from the lids and lashes and into the tear film. One study showed migration of product applied directly to the inner eyelash line migrates onto the ocular surface in as little as five minutes.5
Adherence to proper hygiene practices with cosmetics can be just as important as hygienic contact lens use. Makeup should be replaced at appropriate intervals (mascara every three to six months, liquid and gel eyeliner every six to eight months and eyeliner pencils and powder annually).6 Additionally, if a patient develops symptoms of an eye infection, it is best to remove contact lenses, discontinue makeup wear and replace products after the infection clears.
As clinicians, we also need to do our part to prevent contact lens-related complications when patients are in the office. After years of overwear of a GP lens, this patient required careful slit lamp evaluation with fluorescein staining to check for corneal compromise and evaluate lens fit, upper lid eversion to check for papillary conjunctivitis and corneal topography to monitor disease progression. Corneal warpage can be difficult to detect on anterior topography in corneal GP lens wearers with keratoconus, as both conditions exhibit steepening on anterior topography.
Each patient visit is also a chance to review signs and symptoms of contact lens-related complications. Since our patient had sought care at an emergency room for a previous red eye, and, because we noted signs of previous inflammation, we reminded her we are happy to triage any future red eye concerns.
One easily accessible resource on best practices for all types of contact lens wear and the prevention of complications is a printable handout from the Association of Optometric Contact Lens Educators called “Healthy Gas Permeable Contact Lens Habits” (available at aocle.org/index.php/healthy-gp-cl-habits). We give a copy to new and returning patients as a reminder of the items reviewed during their visit.
Discuss New Technology
This visit also allowed us to introduce the patient to some of the technology our practice has acquired over the last decade—including corneal tomography, tear osmolarity and scleral mapping. GP lenses certainly have their place in management of both the normal and irregular cornea; however, when we verified the difficulties this patient was having, they centered around reduced vision, dry eye symptoms and irritation. We discussed a GP multifocal with an optimized fit and edge profile as an option but ultimately decided on a scleral multifocal with Tangible Hydra-PEG (Tangible Science) to avoid dessication and microtrauma at the limbus and to attempt to reduce the dry eye symptoms.
We recommended she start using lubricating eye drops regularly in each eye as well as a preservative-free, hydrogen-peroxide-based care system for her new lenses.
Ultimately, this patient was excited at the prospect of improved comfort and having her near vision restored. Her visit was a nice reminder that contact lens patients do require annual evaluations, regardless of whether they say they are doing fine or not. Very often, further questioning and an in-office evaluation of the anterior segment reveals problems we have the capability to solve with new (or old) technology.
| 1. Grohe RM, Lebow KA. Vascularized Limbal Keratitis. Int Contact Lens Clin. 1989;16(7):197-209. 2. Zhao Z, Naduvilath T, Flanagan JL, et al. Contact lens deposits, adverse responses and clinical ocular surface parameters. Optom Vis Sci. 2010;87(9):669-74. 3. Boston Simplus Multi Action Solution [package insert]. Bausch + Lomb; 2019. 4. Wu YT, Zhu H, Willcox M, Stapleton F. The effectiveness of various cleaning regimens and current guidelines in contact lens case biofilm removal. Invest Ophthalmol Vis Sci. 2011;52(8):5287-92. 5. Goto T, Zheng X, Gibbon L, Ohashi Y. Cosmetic product migration onto the ocular surface: exacerbation of migration after eyedrop instillation. Cornea. 2010;29(4):400-3. 6. How long does makeup last? Loreal Paris USA. www.lorealparisusa.com/beauty-magazine/makeup/makeup-looks/does-makeup-expire.aspx. Accessed October 2, 2020. |


