 |  |
Several years before the release of the Tear Film and Ocular Surface Society’s (TFOS) Dry Eye Workshop II report, TFOS conducted a separate workshop investigating contact lens discomfort (CLD). Defined as “a condition characterized by episodic or persistent adverse ocular sensations related to lens wear,” CLD can lead to reduced wearing time and eventual discontinuation.1
When patients begin complaining of discomfort, contact lens wear and a multitude of environmental factors may confound the practitioner’s assessment and management strategy for CLD. However, in the absence of evident ocular surface disease, the primary focus is often placed on the contact lens choice. To combat CLD, the most common initial steps include changing contact lens materials, care systems and increasing the lens replacement frequency to a daily disposable modality.
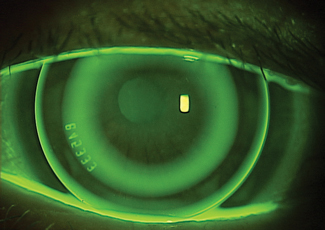 |
| Ortho-K can be a unique option for some patients struggling with contact lens-related discomfort. |
Although seldom considered, orthokeratology (ortho-K) is another viable option to prevent discomfort and subsequent discontinuation of contact lens wear.
Why Ortho-K?
The origins of this modality, also called corneal reshaping or vision shaping treatment, date back to George Jessen’s orthofocus technique in which polymethyl methacrylate lenses were intentionally fit flatter than the corneal curvature to mold the cornea and reduce myopic levels.2 Modern ortho-K lenses now use higher dK gas permeable materials with a reverse geometry design to reshape the anterior cornea. Worn in a closed-eye setting while the patient is asleep, these lenses often temporarily correct refractive error after lens removal.
It seems obvious that ortho-K, which eliminates the need for contact lens wear during waking hours, would effectively mitigate CLD. Several studies have compared the performance of ortho-K with daily soft contact lens (SCL) wear. One early study in 2005 compared ortho-K with hydrogel SCLs and found 67.7% of participants preferring ortho-K to SCLs. When asked about symptoms such as itching, dryness or lens awareness in each modality, ortho-K lenses rated better, even with some patients who preferred SCL wear.3 A similar study using the National Eye Institute Refractive Quality of Life questionnaire also demonstrated decreased ocular symptoms and perceived visual independence with ortho-K wear.4
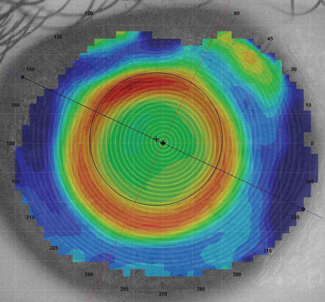 |
| Corneal topography is an essential tool for ensuring proper centration of an ortho-k lens. |
A decade later, researchers more specifically compared dry eye symptoms between ortho-K lenses and newer generation silicone hydrogel (SiHy) SCLs. In one study, both habitual SiHy wearers and neophyte contact lens wearers were fit in ortho-K lenses. Several dry eye indices, including Ocular Surface Disease Index (OSDI), tear break-up time and goblet cell density (GCD), were recorded at baseline and after one month of lens wear. For previous SiHy wearers, the OSDI score improved and GCD increased after only one month of ortho-K lens wear.5
A second study compared both signs and symptoms of ocular dryness between SiHy and ortho-K lens wearers over the course of three months. To assess subjective symptoms, researchers used a dry eye questionnaire to elicit symptoms such as dryness and discomfort. Biomicroscopy helped to evaluate bulbar and limbal redness and conjunctival staining. The results showed that end-of-day discomfort and dryness in the ortho-K group were lower than the SiHy SCL group, with the higher levels of discomfort corresponding to increased redness and conjunctival staining.6
How It Works
In 2002, the Food and Drug Administration approved the first overnight ortho-K lens for the treatment of up to -6.00D of myopia, with or without -1.75D of astigmatism.7 While treatment of low to moderate myopia under -4.00D has a higher rate of success, the off-label treatment of more than -6.00D can be successful.8
| New Modality, New Risks |
| While ortho-K eliminates CLD during waking hours, it comes with its own risks. Proper patient education can go a long way to reduce even these potential problems. Corneal edema and staining are two of the most common side effects, and researchers have noted others such as pain, redness, tearing, irritation, discharge, ocular abrasion or visual distortion.1-3 1. Ladage PM, Yamamoto N, Robertson DM, et al. Pseudomonas aeruginosa corneal binding after 24-hour orthokeratology lens wear. Eye Contact Lens. 2004;30(3):173-8. 2. Young AL, Leung AT, Cheung EY, et al. Orthokeratology lens-related Pseudomonas aeruginosa infectious keratitis. Cornea. 2003;22(3):265-6. 3. Choo JD, Holden BA, Papas EB, Willcox MD. Adhesion of Pseudomonas aeruginosa to orthokeratology and alignment lenses. Optom Vis Sci. 2009;86(2):93-7. |
The original theory, based on Jessen’s orthofocus technique, was the entire cornea would bend and flatten from lens compression.2 Topographical analysis of ortho-K wear does show flattening of the central treatment zone; however, more current research suggests anterior corneal tissue is redistributed with the help of tear film forces.9 The exact mechanism is still debated, but histological studies using a feline model have shown both corneal epithelial cells and anterior stroma undergo change.10,11 As a result, corneal thickness measurements confirm the thinning of the central cornea while the mid-peripheral cornea thickens.9,12
Although widely used for myopia, ortho-K lenses can also be used to treat low levels of hyperopia. Similar to the mechanism for myopia reduction, tear film forces are thought to be involved with corneal reshaping. By fitting the lens steep, the post-lens tear film supposedly creates a suction force inducing central corneal steepening.13 Studies have indicated close to a 1D refractive shift can be expected after one night of wear as a result of central corneal steepening and mid-peripheral flattening.13,14 However, the use of fenestrated lenses without a statistical difference in clinical effect suggests the tear film forces are more likely a compressive force than a suction force.
Ortho-K has maintained popularity thanks to its role in myopia control for children.15 The ability to correct refractive error at night—eliminating the need for daytime lens wear—makes these lenses a great option for patients with low hyperopia and mild presbyopia as well. If patients have struggled with CLD but aren’t fond of spectacle wear, ortho-K may be a viable option if they fall within correctable parameters.
1. Nichols JJ, Willcox MDP, Bron AJ, et al. The TFOS international workshop on contact lens discomfort: Executive summary. Invest Ophthalmol Vis Sci. 2013;54:TFOS7-TFOS13. |


