The process of fitting presbyopia patients with multifocal contact lenses is often fraught with challenges. Some are hesitant to wear them, others are on board with the idea but the choices seem endless. Still more have unrealistic expectations that almost doom the endeavor from the start. And it’s not just the patient who feels overwhelmed; some ODs feel the same way, as there are many anatomical features, optical advantages and patient-specific alternatives to be aware of.
Prospective patients for multifocal lens wear need to have clear optical media, ideally with minimal aberrations or deviations from the norm, given the complexity of the visual correction being attempted in a single design. Anatomical factors impacting the performance of the lens optics include corneal shape (e.g., prolate, elliptical), any dystrophies, pupil size (in scotopic, mesopic and photopic settings), lens crystalline clarity, aberrations and misalignment with the visual axis. Individual patient characteristics include total ocular system spherical aberration, centration and the ability to neuroadapt.1 Posterior segment concerns like epiretinal membrane or any macular disorders also raise the degree of difficulty in fitting multifocals.
Contact lens correction for presbyopia accounts for up to 25 to 35% of contact lens fittings in some countries, though adoption in the United States tends to lag internationla markets.2 Here, we’ll look at the options, impediments and decision-making process to help improve your odds of success in meeting the needs of presbyopes with a contact lens option.
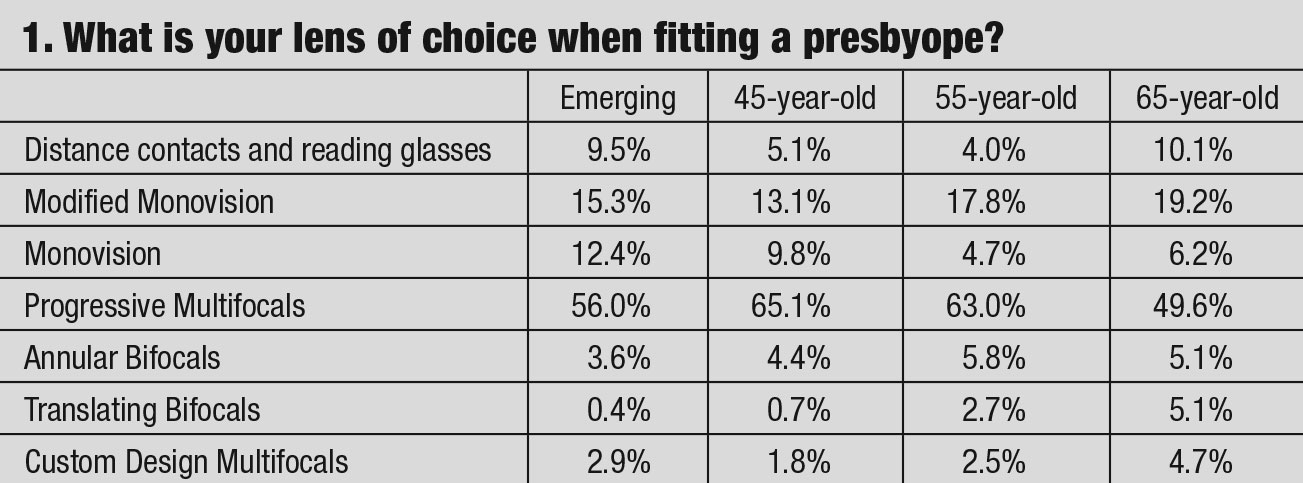
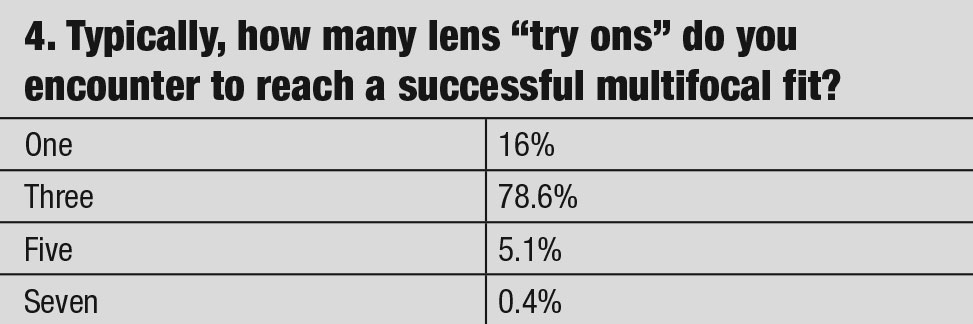
Practitioners investigate the advantages and disadvantages of presbyopic lens designs through patient experience, discussing outcomes with colleagues, reading articles and listening to clinical pearls from speakers. We thought asking the 1,700 members of the American Academy of Optometry’s Cornea, Contact Lens and Refractive Technologies Section for their viewpoints on presbyopia contact lens fitting might give additional insight. The questionnaire’s goal was to examine whether the practitioner’s prescribing habits in correcting presbyopia change with its severity or age. This survey did not look at the different methodologies of fitting advanced cases of post refractive surgeries, corneal anomalies/dystrophies or dry eyes. The questions are shown in the table and answers are discussed below.
 |
| Click table to enlarge. |
Progressive Multifocals
The majority of the responding clinicians’ first lens of choice for the initial diagnosis of presbyopia was a progressive multifocal design. This is due to advancements in the fabricating technology that “eases” the fitting process. Most simultaneous vision multifocal contact lens designs incorporate multiple add powers. The majority of the responding practitioners prefer soft lens designs over hybrid and gas permeable options, owing to patient comfort concerns.
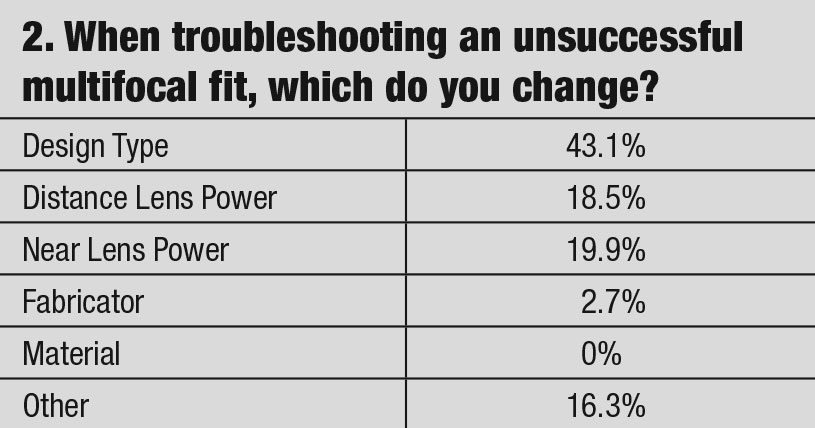
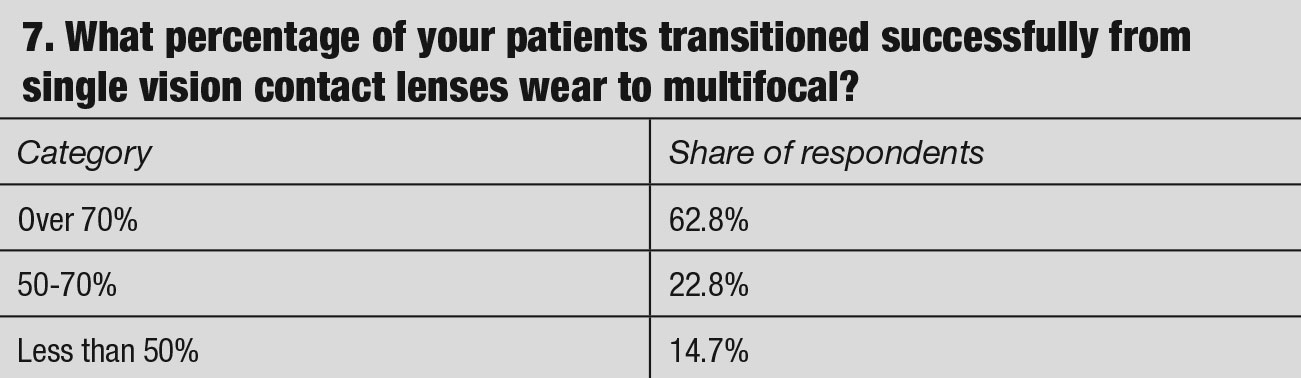
However, even with recent advancements in multifocal lens design, the success rate is still questionable. Only 62.8% of practitioners reported a success rate of 70% in transitioning patients from single vision to multifocal design. Typical reasons why multifocal lenses may have a lower chance of success include relatively restricted lens choices (compared to spherical options), anatomical limitations and visual demands due to lifestyle. While some of the reasons are generally age-related discomfort and problems with handling lenses, dissatisfaction with the performance of multifocal soft lenses due to unwarranted visual compromise does not make it an appealing choice for the presbyopic lens wearer.7
 |
| Click table to enlarge. |
It should be noted that only 29% of contact lens dropouts are presented with other designs and modalities to try.3 Visual change related to advancing age is another factor that causes patients to drop out of contact lenses.4
The advancement of lens production, lens materials and improved understanding of scleral anatomy and physiology have increased the indications for scleral lenses prescribing. Scleral contact lenses designs are regarded as one of the improved correcting solutions for eyes that have failed with traditional lens modalities.5 However, only 5% of respondents’ lens wearers make use of this modality.6 Correcting presbyopia in a scleral lens design is not impossible but may be impractical for mainstream use. While corneal gas permeable refits were prescribed only 8% of the time in our findings, it is still higher than the reported trend of 4%.7
 |
| Click table to enlarge. |
Monovision and Modified Monovision
These choices collectively comprised the second-most selected approach to presbyopic correction in our survey. An interesting pattern resulted with the highest percentage of fits with the emerging presbyopes and patients over 65 years of age. This fitting approach for the emerging presbyope correcting distance vision with the dominant eye and near vision with the non-dominant eye was selected approximately 25% of the time by practitioners. Monovision is advantageous in the early stages of presbyopia, with a prescription gap up to +1.75D between the two eyes in instances when multifocal contact lenses do not achieve ideal vision at both distance and near. Patients over 65 using modified monovision multifocal approach enhanced visual performance, as the dominant eye is corrected for distance with a lower add multifocal power, while the non-dominant eye is corrected with a higher add power.
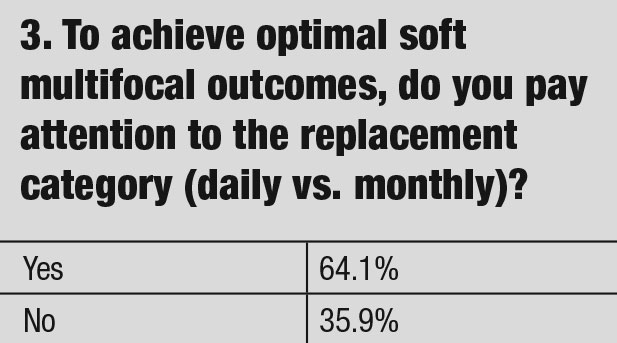
Practitioners fitting presbyopic patients should select the design with the best visual effect and lens comfort that attributes to improved outcomes. Our questionnaire found an interesting trend among practitioners, with 64% paying attention to the replacement category (daily vs. monthly) when fitting presbyopia. This statistic, coupled with almost 14% who define success by the wearing schedule, reveal that practitioners are more concerned with wear schedules than finding a successful lens design—no matter the replacement cycle. To improve contact lens success, the resultant acuity and comfort attributes should be the priority.
 |
| Click table to enlarge. |
Multifocal lens designs are constructed into several categories: center-near aspheric, center-distance aspheric, concentric ring or segmented. The easiest for patients to process information is the segmented design. When they look straight ahead, the visual axis goes through the distance zone; looking down shifts the axis to the reading zone.
In a gas permeable (GP) lens, the lower lid acts as a ledge barrier holding the lens in place as the eyes traverse through the lower reading portion. In the soft version, a new lens to the market incorporates a bump in the upper portion of the lens and uses the upper lid to hold the lens in place as the eyes traverse to the lower bifocal portion of the lens. These lens designs—like spectacles—have the visual system looking through distance in primary gaze and the near portion of the lens when looking through the lower portion of the lens.
 |
| Fig. 1. Bifocal GP lenses offer crisper vision than soft lenses but many patients find adaptation difficult. Click image to enlarge. |
Bifocals
In annular bifocal or aspheric multifocal simultaneous-image correction lenses, light rays pass through the pupil to form the retinal image incorporating distance and near corrections (annular design) or a smooth transition in power between distance and near corrections (aspheric multifocal design). The image on the retina receives both in-focus and out-of-focus images.
 |
| Click table to enlarge. |
One negative outcome of these simultaneous optical lens designs is a reduction of contrast.8,9 The retinal image is degraded by the induced spherical aberration in these designs, but this is countered by the increase in the vergence range over which there is no apparent deterioration in retinal image quality because depth of focus is increased.10–13 The one factor that cannot be controlled is the difference between individual patients in their tolerance of blur, which may be attributed to inherent optical factors, such as pupil size, higher-order ocular aberrations and binocular summation.14-18
The simultaneous vision category divides the pupil area designated for near and distance zones. It is this balance that will determine patient acceptance to the lens design. Pupil size controls the amount of the two images focusing on the retina, and power only controls where the image is focused or working distance.
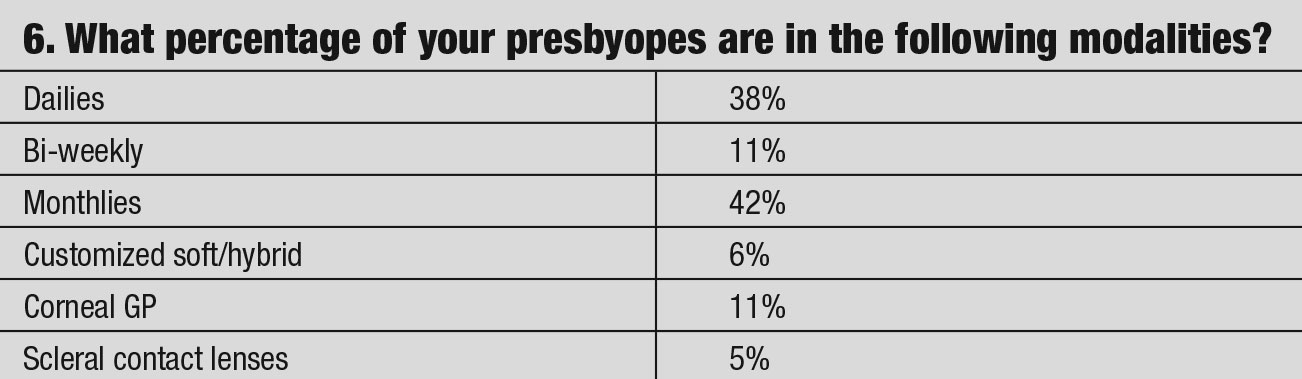 |
| Click table to enlarge. |
Progressive Lens Multifocals
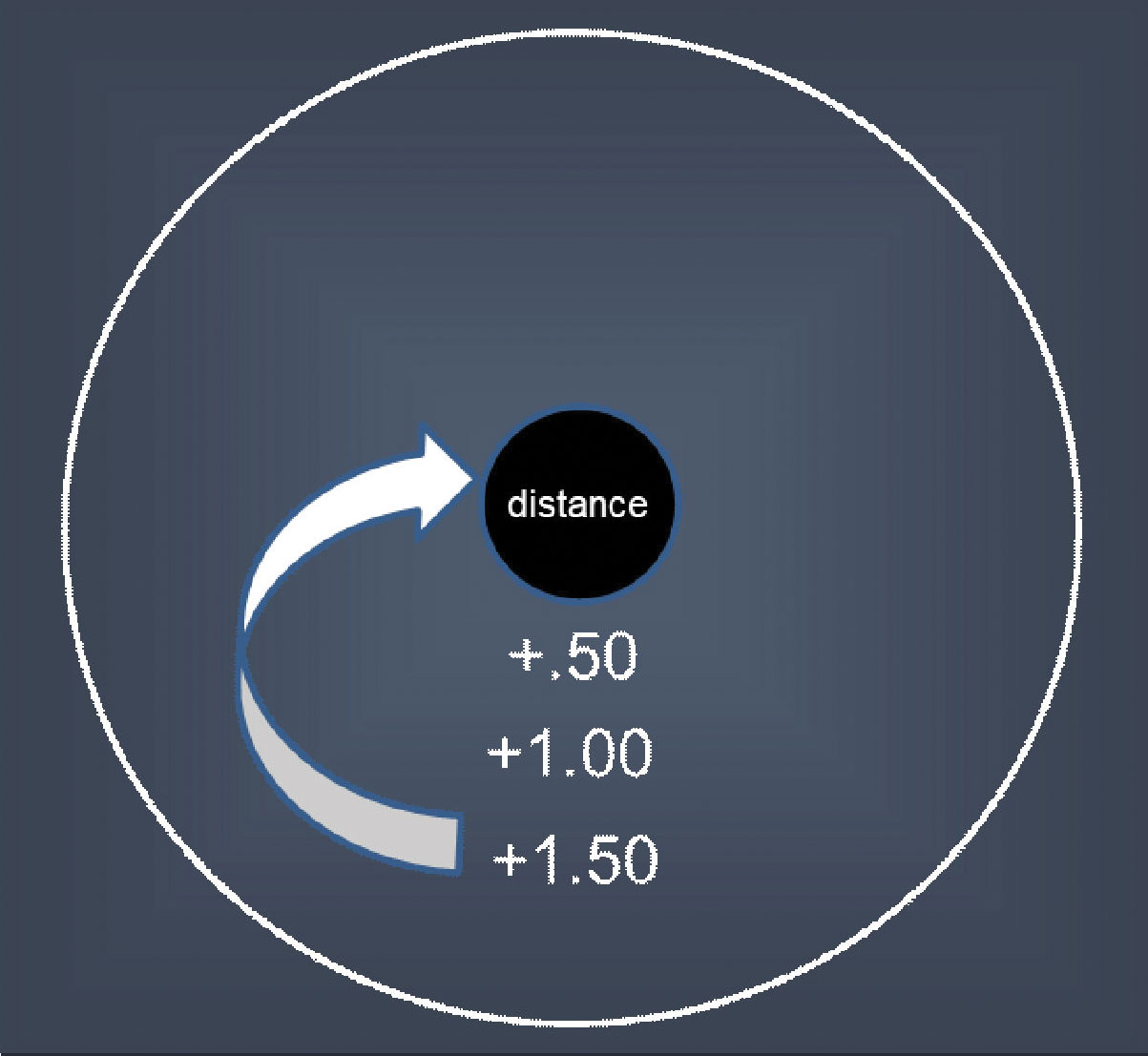
The progressive center-near design has most plus in the center and gradually reduces plus to the periphery; these lenses tend to be more successful with higher add requirements. The progressive distance center lens has most minus in the center and gradually increases in plus in the periphery. Patients with lower add prescriptions adapt to these lens designs quickly because of their similarity to distance-only lens designs.
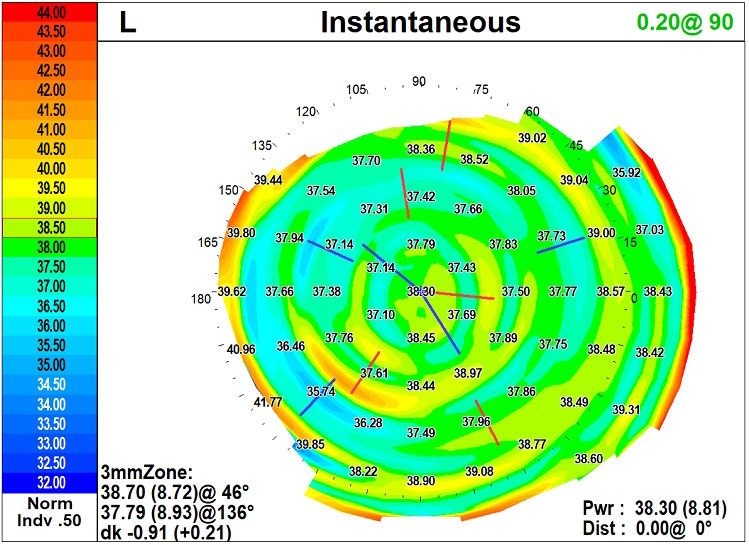 |
| Fig. 2. Corneal topography performed over a multifocal. Click image to enlarge. |
The concentric ring design alternates near and distance zones within the pupil area. The power distribution across the lens is highly dependent on pupil size variations, line of sight and lens centration to provide a positive visual effect for presbyopia; patients take a little more time to adapt to this design.
An additional multifocal lens design uses the annular concept in the center zone and periphery zone while incorporating the progressive design as the transition between the two annular zones, and creates a customized multifocal. A problem inherent to all multifocals: as the power distribution is divided between near and far, visual range contrast sensitivity is reduced. The goal is to provide a balance between the defocused image without compromising the focused image. As patients age and pupils become smaller, depth of field increases, which will improve multifocal contact lens performance.19
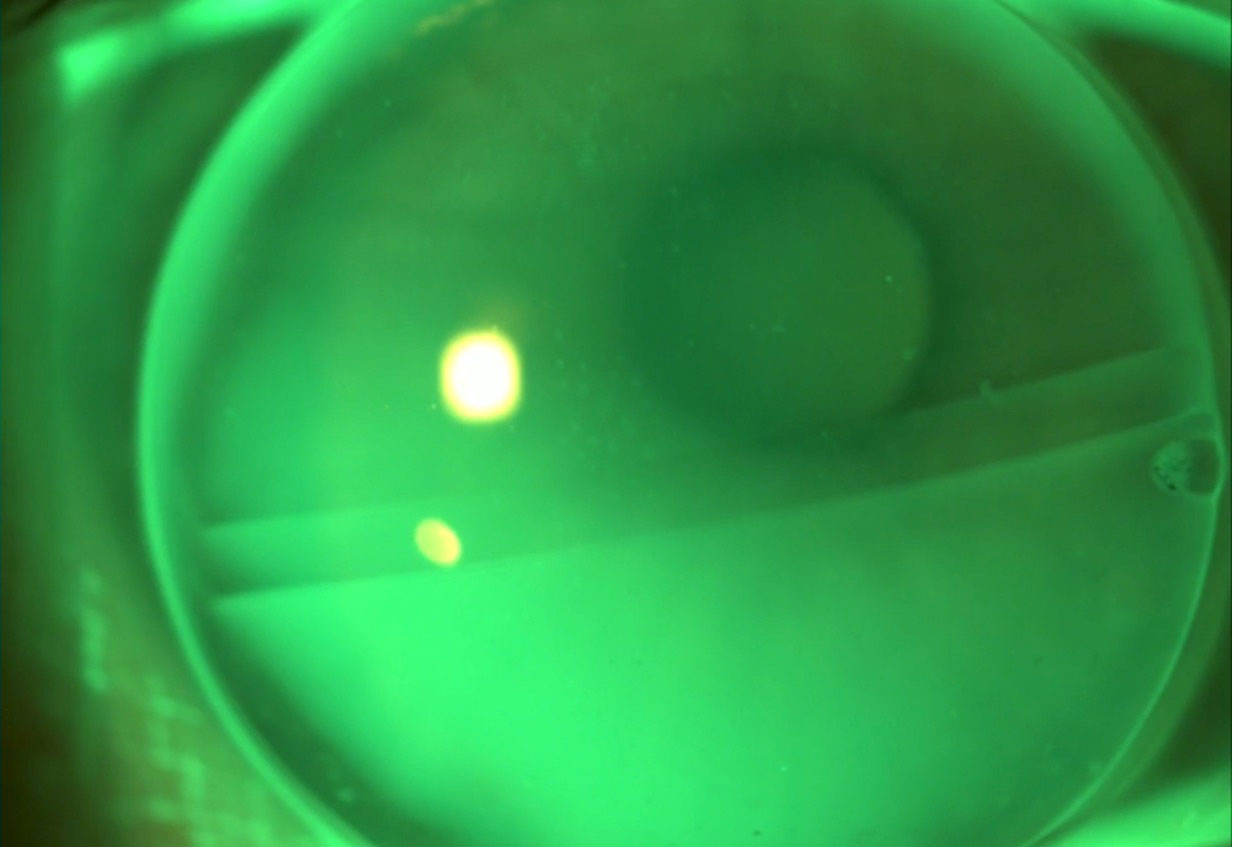 |
| Fig. 3. Anterior segment image of a fluorescein pattern of a trifocal GP contact lens. Click image to enlarge. |
The Best Fit
Fitting multifocal/bifocal lenses can be broken up into distinct stages. The first is deciding the power configuration, the second is creating a perfect centered-lens design and the third is neutralizing ocular aberration and aligning the image onto the fovea. Once these factors are engineered into a lens design, the patient will respond with real-world feedback, giving additional insight that can lead the practitioner toward a successful outcome.
The total power configuration (near, intermediate and distance) has to reside within the pupil. If any portion of the power zone falls outside the pupil, clarity will be affected. This visual aperture is also changing determined by the amount of illumination. The outcome is dependent on the percentage of distance vs. near power within pupillary area, whether it is center-near or center-distance design.
All power zones must reside within the space designated by the pupil. In either a distance-centered or a near-centered lens, the surrounding power always has a negative effect on visual outcome, reducing contrast sensitivity. As the power of the surround increases, the effect is magnified.
 |
| Click table to enlarge. |
If a patient has a 4.0mm pupil under photopic conditions and the lens design incorporates 2.2mm near center zone, then 1.8mm is left for the distance zone. To improve near vision, the only alternative is to increase the space of the near zone to 2.5mm—leaving 1.5mm for distance. The doctor-patient relationship entails trying to partner and balance these zones to arrive at a mutually successful result. Increasing the near prescription only reduces the working distance and does not improve vision quality. Patients with small pupils require a smaller central optical zone in order to incorporate the surround.20 These patients tend to perform better with a distance-centered optics. Using a smaller central optical zone will minimize the visual deterioration from spherical aberration while improving extended depth of focus (EDOF). These can be fabricated akin to a variety of optical philosophies seen in the IOL market.
EDOF and diffractive concepts use spherical aberration and chromatic aberration to enhance the multifocality and contrast sensitivity of these designs. Positive spherical aberration focuses marginal rays in front of the retina and paraxial central rays are focused on the retina, while negative spherical aberration focuses marginal rays behind the retina and central rays on the retina. It is the difference between these foci that result in depth of field.
By manipulating the degree of positive and negative spherical aberration, a superior lens design is created; whereas the diffractive design uses a wavelength of color to create different foci.21 These different foci create a diffractive lens design to minimize chromatic aberrations, resulting in an improvement in contrast sensitivity and quality of vision.22-23 Both of these optical techniques are affected by pupil size, which is why multifocal contact lenses perform differently during changes in illumination between patients.
 |
| Thickened superior area for stabilizing a translating soft lens. Click image to enlarge. |
Custom Design Multifocals
Correcting the visual system for higher-order aberrations is contingent on perfect centration and non-rotating lens designs. Manipulating the lens parameters and at times decentering the optics creates the optimal system. In order to successfully develop the necessary fitting parameters at times, custom lens designs are necessary to accomplish the task. Using corneal topography can help in the determination of centration and accurate optical alignment of the contact lens. Integrating this technology into routine contact lens care will help manipulate lens parameters to eliminate some potential optical inaccuracies and improve visual outcomes.
One of the most difficult challenges that clinicians face when transitioning from single vision contact lenses to multifocal designs is patients’ willingness (or unwillingness) to consider a temporary reduction in their quality of vision. Therefore, early intervention is critical to “easing” them into a new reality of simultaneous vision. This must be presented to emerging presbyopes with a design that has a center-distance prescription. These emerging patients require only a low add, so the power shift will not overwhelm their visual system.
The center-distance design works best with an add power up to +1.75, which corresponds to patients in their late forties. As the add power need increases, so does the gap between their distance and near powers. A progressive multifocal center-near design encompasses a softer transition for those who require increased add powers. At times we have to modify the transition phase from center-distance to center-near correcting the dominant eye with center-distance and non-dominant eye with center-near. It is critical to match visual demands with different multifocal designs; patients who use desktop computers would require a larger intermediate zone whereas those with high near demands would require a larger near zone diameter.
 |
| The surround powers always have a negative effect on central vision. Click image to enlarge. |
As clinicians, we cannot lose sight of the realization that many presbyopes would like to have the flexibility to use contact lenses for certain tasks and glasses for others. However, this growing population is increasingly active and benefits from the visual freedom of being spectacle-free for many of their activities.
According to the United Nations Department of Economic and Social Affairs, the global presbyopic population is increasing, with more than two billion people over the age of 60 expected by 2050.24 Therefore, the prescribing process should not be approached as all-or-nothing situation. This demographic is significantly more engaged and will benefit from the visual freedom of not wearing spectacles nearly as much. Clinicians may help their patients find relief through presbyopia correction by holding thorough discussions before lens fittings, recognizing the different lens designs and being prepared to troubleshoot when patients struggle with adaptation and anatomical or lifestyle challenges.
1. Plainis S, Atchison DA, Charman WN. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013; 90(10):1066-77. 2. Bennett ES. Contact lens correction of presbyopia. Clin Exp Optom. 2008; 91(3): 265-78. 3. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40(1):15–24. 4. Pucker AD, Jones-Jordan LA, Marx S, et al. Clinical factors associated with contact lens dropout. Cont Lens Anterior Eye. 2019;42(3):318–24. 5. van der Worp E, Johns L, Barnett M. Scleral schism. Cont Lens Anterior Eye. 2019;42(1):1–2. 6. Nichols JJ, Fisher D. Contact lenses 2018. Contact Lens Spectrum. 2019;34:18–23. 7. Akerman DH. 40 is the New 20/20—presbyopia equals opportunity. Contact Lens Spectrum. 2010;25:3. 8. Charman WN, Saunders B. Theoretical and practical factors influencing the optical performance of contact lenses for the presbyope. J Brit Cont Lens Assn. 1990;13:67–75. 9. Charman WN, Walsh G. Retinal images with centred aspheric varifocal contact lenses. Int Cont Lens Clinic. 1988; 15:87–93. 10. Bakaraju RC, Ehrmann K, Ho A, et al. Inherent ocular spherical aberration and multifocal contact lens optical performance. Optom Vis Sci. 2010;87(12):1009–22. 11. Montes-Mico´ R, Madrid-Costa D, Radhakrishnan H, et al. Accommodative functions with multifocal contact lenses: a pilot study. Optom Vis Sci. 2011; 88(8):998–1004. 12. Rajagopalan AS, Bennett ES, Lakshminarayanan V. Visual performance of subjects wearing presbyopic contact lenses. Optom Vis Sci. 2006;83:(8):611–15. 13. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci. 2006;83(5):266–73. 14. Woods RL, Colvin CR, Vera-Diaz FA, et al. A relationship between tolerance of blur and personality. Invest Ophthalmol Vis Sci. 2010;51(11):6077–82. 15. Bradley A, Abdul Rahman H, Soni PS, et al. Effects of target distance and pupil size on letter contrast sensitivity with simultaneous vision bifocal contact lenses. Optom Vis Sci. 1993;70:(6):476–81. 16. Bakaraju RC, Ehrmann K, Falk D, et al. Optical performance of multifocal soft contact lenses via a singlepass method. Optom Vis Sci. 2012;89(8):1107–18. 17. Ruiz-Alcocer J, Madrid-Costa D, Radhakrishnan H, et al. Changes in accommodation and ocular aberration with simultaneous vision multifocal contact lenses. Eye Contact Lens. 2012;38(5):288–94. 18. Plainis S, Petratou D, Giannakopoulou T, et al. Binocular summation improves performance to defocus-induced blur. Invest Ophthalmol Vis Sci. 2011;52:2784–89. 19. Charman WN, Developments in the correction of presbyopia I: spectacle and contact lenses. Ophthalmic Physoi Opt. 2014;34(1):8-29. 20. Plainis S, Ntzilepis G, Atchison DA, et al. Through-focus performance with multifocal contact lenses: effect of binocularity, pupil diameter and inherent ocular aberrations. Ophthalmic Physiol Opt. 2013;33(1):2–50. 21. Rocha KM, Gouvea L, Waring GO 4th, Haddad J. Static and dynamic factors associated with extended depth of focus in monofocal intraocular lenses. Am J Ophthalmol. 2020;216:271-82. 22. Artal P, Manzanera S, Piers P, Weeber H. Visual effect of the combined correction of spherical and longitudinal chromatic aberrations. Opt Express. 2010;18(2):1637-48. 23. Breyer DRH, Kaymak H, Ax T, et al. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339-49. 24. B.A. Holden, T.R. Fricke, D.A. Wilson, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 25. Morgan PB, Woods CA, Tranoudis IG, et al. International Contact Lens Prescribing in 2020. Contact Lens Spectrum. 2021. |


