Patients perceive eye care practices that utilize state-of-the-art equipment as more current and believe that they are receiving a higher quality of care. Along with the clinical advantages of high-tech equipment, instilling this perception in your patients will set you apart from your neighborhood colleagues. And, through increased referrals and higher billing, technology can improve your bottom line.
So, how do you choose which diagnostic and treatment tools you should add to your high-tech practice? There are a number of equipment options for the anterior segment practice. These include corneal topography, slit lamp optical coherence tomography (SL-OCT), aberrometers, pachymeters, auto refracting systems, specular microscopy and slit lamp cameras. But, what is right for you—and when should you invest?
Corneal Topography
What Can Investing in Anterior Segment Technology Gain You?
• The ability to collect more thorough clinical information about your patients.
• Better patient management.
• More accurate diagnosis.
• Quantitative documentation over time.
• Evaluation of treatment plans.
• Simplified contact lens fittings.
• Improved patient education.
• Easy communication with other practitioners.
• More efficient examination.
• Differentiating yourself from the rest of the market.
• Improving patient perception about the quality of care received.
• Word-of-mouth referrals.
• Increased income.
Corneal topography is fast becoming the standard of care for corneal measurements. This technology aids in patient education, medical and legal documentation, diagnosis, following change over time, contact lens fitting and communication with colleagues.
There are two types of topography systems on the market—projection-based and reflection-based systems. Reflection-based systems assume the cornea behaves as a mirror. A placido disc reflects rings off the corneal surface, and the distance between the reflected rings is recorded. Changes in ring distance represent changes in curvature. These systems are limited, however, when the cornea is non reflective, such as in cases of disrupted epithelium, scarring or dry eye. Keep in mind that elevation data is calculated, which means that there may be an inherent error.
Projection-based systems are appropriate for high-volume anterior segment practices. These systems transmit light through the cornea. Because they do not need a reflective surface, projection-based topographers can obtain measurements on badly distorted surfaces. These systems measure elevation by locating actual points in space through triangulation. In addition to front surface curvature values and elevations, projection- based systems also measure the posterior cornea. These systems can also calculate pachymetry values, angle measurements, epithelium and LASIK flap measurements and phakic IOL vault measurements and aid the practitioner in crystalline lens assessment, shunt and implant imaging, foreign body documentation, surgical pathology and scar monitoring, and contact lens fitting. These instruments carry a hefty price tag, but they are well worth the price to the serious anterior segment specialist. Placido imaging systems are more affordable and are adequate for most practices.
Corneal topography is well understood by the insurance industry, and there are numerous diagnostic codes that support its use. To bill for corneal topography, use 92025, keeping in mind that it is defined as unilateral or bilateral and requires an interpretation and report in the medical record.
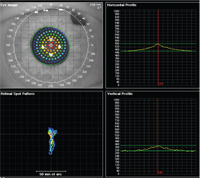
Wavefront abberometry in this Fuch’s dystrophy patient shows significant lower-order abberations.
Anterior Segment Optical Coherence Tomography (AS-OCT)
Anterior segment Optical Coherence Tomography (AS-OCT) is a non-contact instrument that creates three-dimensional, in vivo, cross sectional images of the cornea, lens, iris/ciliary body and adjacent conjunctiva. Its clinical applications include glaucoma and iris/angle examination, corneal imaging for infection, pathology, injury, dystrophies/ degenerations, contact lens evaluations, as well and pre- and post-surgical exams.
The AS-OCT has distinct advantages to ultrasound—which has been the standard of care for decades for ocular structure imaging—including no contact between the instrument and the eye and high-resolution images. When billing for AS-OCT, you can use the HCPCS Level III code 0187T for high-resolution anterior segment ultrasound. A level III code means that while you submit the code to the carrier, the patient pays for the procedure. Level III codes are typically used for tracking utilization of new technologies/procedures and are generally not paid by the carrier.
Aberrometers
Aberrometers use wavefront technology to objectively measure the overall refractive errors of the eye. Once considered just a research tool, abberometers are making their way into clinical practice—especially since the advent of combined corneal topographer/abberometers. These tools are useful in the diagnosis of corneal pathology (such as early keratoconus where coma may show before other clinical signs), refractive surgery evaluations and custom ablations, post-surgical monitoring and superior optical evaluation and designs (glasses and contact lenses).
Hartmann-Shack is the most commonly used wavefront technology in abberometers today. This method relies on the projection of a point source light on the retina. The light reflected from this point on the retina is imaged onto a lenslet array and sampled with a charged coupled device chip. Wavefront aberrations are calculated assuming that a point of light on the retina was the origin of the image. Using a single scan, it offers quick, yet repeatable high-resolution evaluations.
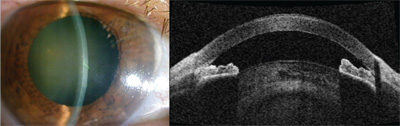
SL-OCT clearly shows swelling and opacity of the cornea, shallow anterior chamber and narrow angles.
Ray tracing is the other commercially available technology; it takes over 256 sampling points within 0.06 seconds in a pupil as small as 2mm. The laser ray tracing technique projects a thin infrared laser beam onto the retina and detects the location of reflection one by one in succession. The merit of this technique is that it can detect larger-magnitude errors of reflection than the Hartmann-Shack method and is not as affected by eye movement.
Hartmann-Shack aberrometers vary in their degree of accuracy, dynamic range, max/min pupil diameters, analysis features and compatibility with other devices. Accuracy and dynamic range seem to be two of the most important factors when choosing an aberrometer. Accuracy corresponds to the number and spread of points measured: the higher the number of points, the better—but the spread must be even. Dynamic range corresponds to the device’s ability to detect the higher and lower ranges as well as the subtleties in variations.1 Less precise wavefront sensors may not detect disorders such as keratoconus, corneal scarring and severe high-order aberrations.
High-frequency ultrasound of the angle, iris and ciliary body—open angles (top), plateau iris (bottom).
Some manufacturers use software interpolation to enhance the optical resolution of the wavefront sensors. Instead of physically measuring each point, the computer takes data from nearby points to calculate and approximate the measurement, allowing more room for error.
There is no CPT code for aberrometry. Therefore use either code 92499 (unlisted ophthalmological service or procedure), which carries a host of billing headaches, or 92015 (determination of refractive state), which is not covered by Medicare and is generally paid out of pocket.
| Questions you need to ask yourself when you are considering adding diagnostic or treatment equipment to your practice:
|
| • How often will I use this machine?
• Can I bill for this? Is this code typically covered by third-party medical carriers? • Is there patient demand for this product? • Will I receive referrals for this service from outside doctors? • How do I market this technology? • How much will it cost in staff time (training)? • What is the advantage of purchase vs. lease, and what are the tax ramifications? • What is my return on investment? • Do I need it to practice or to set myself apart from others? • Is it a research tool? |
Confocal microscopy allows for high-resolution, reliable, real-time imaging of the living corneal microstructure, including normal corneal morphology, pathogen invasion, dystrophies and degenerations, post-surgical management, dry eye, drug toxicities, endothelial monitoring and contact lens-related changes. For a cornea-based practice, confocal microscopy is indispensible in diagnosing and monitoring progression of disease or response to treatment.
There are two commercially available confocal microscopes: the Confoscan 4 (Nidek) is a scanning slit confocal microscope. The Heidelberg Retina Tomographer Rostock Cornea Module (HRT-RCM) (Heidelberg Engineering) is a laser scanning confocal microscope.
A scanning slit confocal microscope uses white light and two optically conjugate slits for illumination for detection of reflected light. This allows for many points to be scanned in parallel, resulting in reduced scan time vs. spot illumination. A scanning laser uses a single wavelength of coherent light as the illumination light source, which scans sequentially over the examination area, offering high-depth resolution. The scanning laser technique can also evaluate the conjunctiva, sclera, limbus, lid, lacrimal gland and tear film.
The Confoscan 4 is a standalone unit, while the HRT-RCM is an attachment to the Heidelberg Retinal Tomographer.
There are three codes that may be used for confocal microscopy: endothelial cell counts (92286), external ocular photography (92285) and optical corneal pachymetry (92499).
External photography is billable to insurance if it’s medically necessary and the procedure is needed to diagnose, treat or monitor treatment of the patient’s condition. Confocal microscopy cannot be billed for documentation of a healthy eye.
Pachymetry for glaucoma is generally only covered by insurance bilaterally once per lifetime using code 76514; however, pachymetry associated with corneal pathology—such as keratoconus, endothelial disease or corneal transplantation—may be covered based on medical necessity.
Specular Microscope
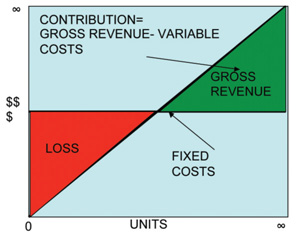
These simple calculations tell you whether making that purchase now will help or hurt your bottom line.
Specular reflection occurs when light is reflected at the interface of materials with different refractive indices and when the angle of incidence is equal to the angle of reflection. In the cornea, the endothelial cells have a different index of refraction than the underlying aqueous and the overlying Descemet’s membrane. So, in specular microscopy, light reflected backward is used to form an image of these structures.
Specular microscopy, or endothelial imaging, allows for the evaluation of endothelial cell density, polymegathism and pleomorphism. These factors are useful for evaluating injury, disease such as Fuch’s or Posterior Polymorphous Dystrophies, post-surgical conditions such as penetrating or endothelial keratoplasties, inflammation or changes due to contact lens wear.
There are several endothelial-imaging devices on the market today, including dedicated cameras and confocal instruments. The code for endothelial cell photography is 92286.
Endothelial photography is reimbursable when it is reasonable and necessary. Eligible patients must meet one of the following criteria; they must:
• Show evidence of endothelial dystrophy (guttata).
• Have corneal edema.
• Be about to undergo a secondary IOL implantation.
• Have had intraocular surgery and now require cataract surgery.
• Be about to undergo surgery with a high-risk endothelium.
• Show evidence of posterior polymorphous dystrophy or iridocorneal-endothelium (ICE) syndrome.
• Be about to be fitted with an extended wear contact lens after intraocular surgery.2
Pachymetry
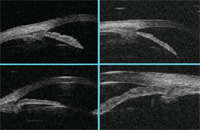
Corneal pachymetry is the measurement of corneal thickness and can be done by either ultrasound or optical pachymeters. Optical pachymeters include confocal microscopy, scanning slit topography, specular microscopy and anterior segment optical coherence tomography. In ultrasound pachymeters, considered the gold standard, ultrasonic energy is emitted from the probe tip, which acts as both transmitter and receiver. The energy is reflected back in the form of an echo. Measurement data is calculated based on the time it takes for the echo to travel back to the probe and the present velocity.
The CPT code to use is 76514 (determination of corneal thickness by ultrasound) unilateral or bilateral. Pachymetry is a payable procedure for any condition that is known to change corneal thickness, such as bullous keratopathy, Fuch’s dystrophy or keratoconus. It is also payable for a glaucoma suspect if it has not been previously performed. But, many insurance plans specifically exclude coverage for refractive surgery.
Slit Lamp Photography

Slit lamp-mounted digital cameras help practitioners to monitor disease progression and treatment efficacy; they are also a key tool in communicating with other practitioners and labs.
Anterior segment photography is a must-have in today’s anterior segment practice. There are a multitude of benefits to taking pictures, but the main reason to use anterior segment photography is for medical and legal documentation. Photos are crucial for monitoring lesions, following for progression. And, evaluating treatment efficacy, and photography can be billed to the patients’ insurance. Photos also enhance patient education, communication with other doctors or labs, prosthetic contact lens color matching and documentation of ocular motility deviations.
There are many choices when it comes to choosing a camera. Slit lamp-mounted digital cameras offer excellent image quality. They have many optimal features including footswitch image capture (for hands-free photography,) halogen illumination and digital video freeze, which pulls still photos out of video. Video freeze is helpful when the patient is moving or blinking. Slit lamp mounted cameras can be hooked up to chair-side computers for instant patient viewing and easy download to patient medical records or photographic databases. The downside to slit lamp mounted technology is its lack of portability and cost. Alternatively, hand-held mini digital cameras are extremely portable and inexpensive. So, how do you manage all the images that you will accumulate over time? Photos should be stored in a patient database and backed up regularly, so an image management system is recommended. Some electronic medical record systems allow photos to be linked directly to the patient record. When setting up a database, make sure that it is HIPAA compliant.
The CPT code for slit lamp photography or external photography is 92285. External photography is billable to insurance if it is medically necessary and the procedure is needed to diagnose, treat or monitor treatment of the patient’s condition. Photos for prosthetic color matching and communication with labs may not meet the medical documentation requirement and are generally paid for out of pocket.
A Sound Financial Investment?
You know that investing in capital equipment is necessary to maintain a vital anterior segment practice. But, how do you decide whether you can really afford that new piece of technology? How much revenue must you earn to cover the cost—and exactly how many more patients you need to see to bring in that revenue?
• Revenue per patient is simply the average amount each patient pays you. To determine your revenue per patient, divide your gross collected income by the number of revenue-generating unique patient visits for that year. So, if your practice had a gross income of $550,000 in 2009, and you performed 2,300 (revenue generating) visits, your revenue per patient is $239.
• The other calculation that is necessary for evaluating a capital equipment purchase is contribution margin, or the fraction of sales that contributes to the offset costs. There are fixed costs (equipment tends to be a relatively fixed cost) and variable costs, such as supplies or extra technical support to run the equipment. Revenue from a piece of equipment must pay your fixed expenses and your variable expenses. When fixed expenses are paid, you’ve reached the break-even point. From then on, the revenue generated only has to cover variable costs. After variable costs are covered, the rest is profit.
Gross revenue minus your variable costs is your contribution. For example, if gross revenue for a corneal topographer is $48,000, and you subract variable costs of 10%, for paper and electricity ($4,800), this results in a contribution of $43,200. To obtain your percentage contribution margin, divide your contribution by your gross income. In this case, that would be $43,200 divided by $48,000, which works out to 0.90 or 90%.
Determining Associated Costs
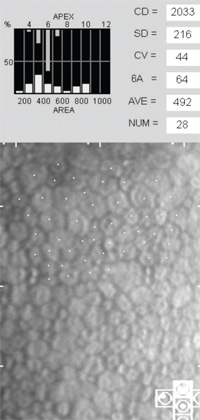
Polymegathism and pleomorphism in a low-Dk contact lens wearer.
When you know your per-patient revenue and your contribution margin, you can put these figures to work. For instance, if you want to purchase a $25,000 topographer, you must figure in not only the cost of the product, but also fixed and variable costs associated with it. Contribution margin helps you to determine how much new revenue you need to cover the cost of adding a fixed expense and the variable costs associated with it. Assuming a contribution margin of 90%, how much additional income must you generate to cover the expenses of a $25,000 corneal topographer? Divide the cost of the equipment, $25,000, by your contribution margin, 90%, which equals $27,778.
Evaluating a Purchase
Now that you know that you need $27,778 to cover the new topographer and associated expenses, you need a plan that will help you increase your gross income by that much. That’s where you’ll use your revenue per patient.
You already know your average revenue per patient is $239. So, if you see 25 new contact lens patients a month and charge $40 per topography, ($239 exam + $40 topo = $279 x 25 patients = $6,975 per month or $83,700 per year), this is more than enough to cover the cost of the $27,778.
The same method works for leasing equipment, too. Instead of using the purchase price, use the annual lease cost. Make sure you include any added costs that come with the lease, such as additional property insurance you may be required to carry.
Proper Planning
Investing in capital equipment is necessary for healthy practice growth. But, you can’t just start buying every piece of high-tech equipment out there—you must first conduct extensive research and calculations to determine the right products and financial investments for you, your patients and your practice. Once you have all the preliminaries squared away, you can have your pick of the many high-tech options available to ensure that yours is the best- dressed anterior segment practice in town.
1. Wu P, Liu S, DeHoog E, Schwiegerling J. Systematic errors analysis for a large dynamic range aberrometer based on aberration theory.Appl Opt. 2009 Nov 10;48(32):6324-31.
2. Medicare National Coverage Determinations Manual. Available at: www.cms.hhs.gov/manuals/downloads/ncd103c1_part1.pdf. (Accessed August 2010).


