 |
Incredibly, I saw two patients with heavily deposited lenses in back-to-back appointments on the same day. Each one was fairly asymptomatic and overdue for an annual exam.
The importance of regular lens replacement and proper cleaning, as well as annual visits to reinforce these procedures, is critical to ensure patients can maintain clear vision and continue contact lens wear without complications. One goal of contact lens management is prevention of unwanted changes to the anterior segment that could affect vision and comfort.
Case One
 |
|
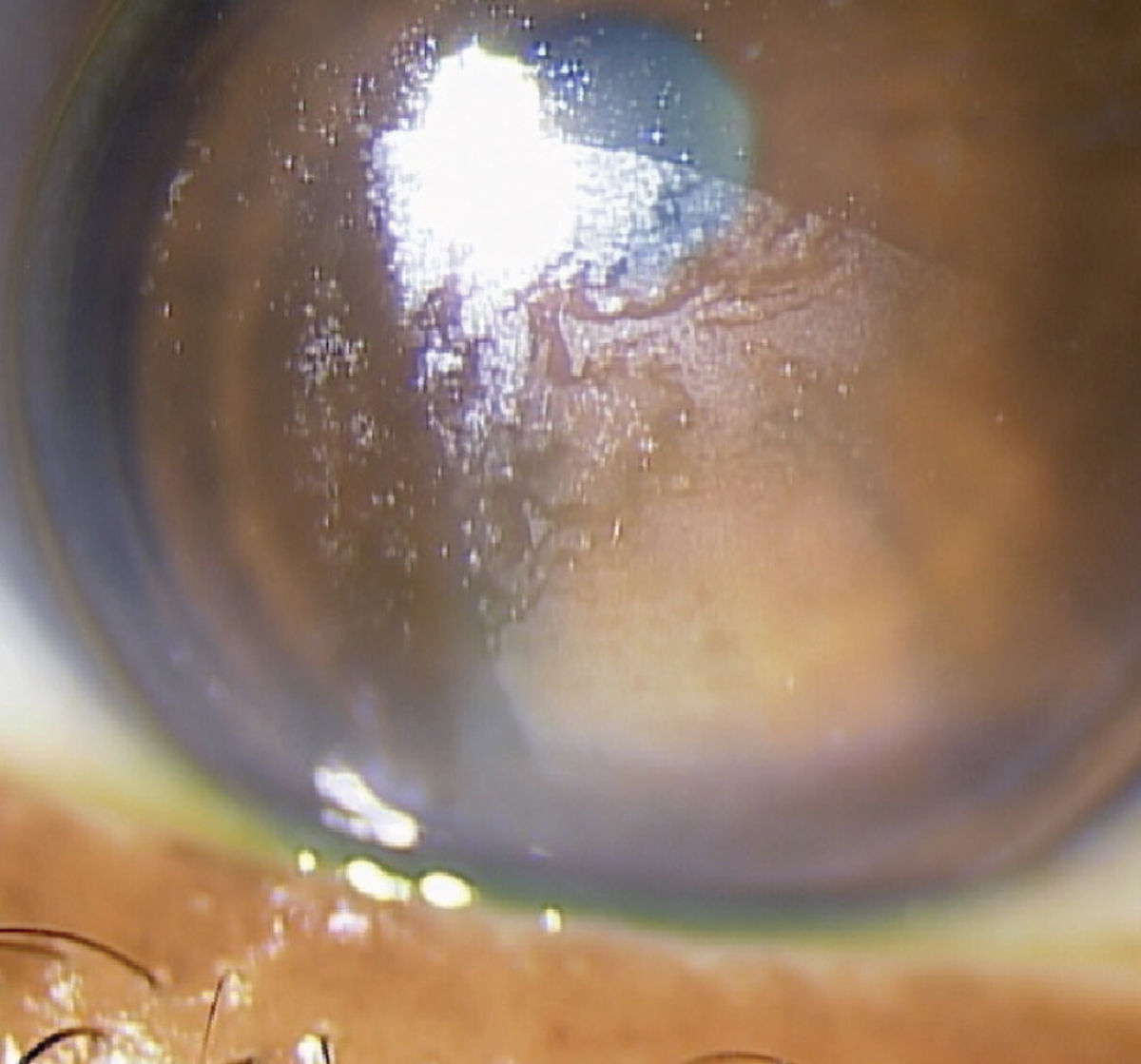
Fig. 1. Corneal lens with acquired mucoprotein film on the anterior lens surface in case one patient. Her incomplete blink pattern is evident, as the upper third of the lens is more clear. Click image to enlarge. |
A 58-year-old female presented wearing the same corneal lenses for the past three years reporting good, stable vision. Her last eye exam was one year ago at an outside practice where she purchased updated spectacles but did not bring her lenses for evaluation. She is using +1.75DS over-the-counter readers over the lenses for near and wears the lenses 12 to 14 hours per day. She notes that she has some irritation at the end of the day, which is relieved with lens removal. Solutions include Boston Advance Comfort (Bausch + Lomb) and weekly Boston one-step liquid enzymatic cleaner (Bausch + Lomb).
The patient also complains of itching of eyelids and associated dryness symptoms that have been occurring for over two years. She reports the dryness and itching are relieved with artificial tears and azelastine as needed. She has a history of lattice degeneration OU with a round retinal hole OS without elevation or subretinal fluid. She also has chronic allergic conjunctivitis and dry eye OU. She is taking flaxseed oil and a variety of vitamins.
Entering VA was 20/20 in each eye. The patient’s habitual GP lenses are OD 7.40/9.0/-8.25DS and OS 7.40/9.0/-8.75DS corneal lenses in Boston XO2, a third-generation fluorosilicone acrylate (FSA) material with a Dk of 141. The fit was lid-attached OD and more interpalpebral OS. There was evidence of incomplete blinking in each eye consistent with the pattern of deposits. The fluorescein pattern showed apical alignment and adequate mid-peripheral bearing in each eye with good centration and movement. The patient accepted an over-refraction of +0.75DS over each eye.
Each corneal lens demonstrated an acquired mucoprotein film over the anterior lens surface, causing a hazy appearance (Figure 1). Typically, this film develops over several weeks or months of wear. The deposits can be caused by a variety of factors including poor tear quality, improper blinking, inadequate compliance with lens replacement or solution use, foreign contaminants (such as residue not removed by proper handwashing practices), surface scratches and poor surface wetting.2 When tear film quality is poor, its continuity over the lens surface is not maintained and lens surfaces become dry. This allows for the formation of deposits on the lens—sites where protein and lipids can become attached to the lens, causing discomfort and reduced wearing time for the patient.3
There was trace fluorescein staining nasal and temporal OD and temporal and inferior OS on the cornea after lens removal. The tear break-up time was instant in each eye. The most recent refraction was relatively stable to previous visits at OD -7.75 -1.50 x 155 and OS -7.75 -1.00 x 160 with a BCVA of 20/20 in each eye. The spectacle add was +2.25DS. The dilated fundus evaluation revealed stable findings OU.
The lenses were cleaned in-office with Boston Laboratory Lens Cleaner (Bausch + Lomb) and the patient was advised to replace the lenses. In addition, it was recommended she continue using Boston Advance Comfort two-step cleaning system as it is specifically designed for FSA lenses, which are more prone to lipid deposits.2 The patient was also asked to continue weekly use of the one-step preservative-free liquid enzymatic cleaner containing subtilisin (a proteolytic enzyme) and glycerol.3
She was advised to continue using contact lens-compatible rewetting drops QID OU and was switched from generic azelastine to olopatadine 0.7% ophthalmic solution (Pataday Extra Strength, Alcon) once each morning in both eyes. We also discussed blink exercises and the need to return within one month for further dry eye evaluation in order to consider additional treatment options. New lenses were ordered. The plus over-refraction was not incorporated into the new lenses due to the deposits; however, it should be re-checked once new lenses are dispensed.
 |
|
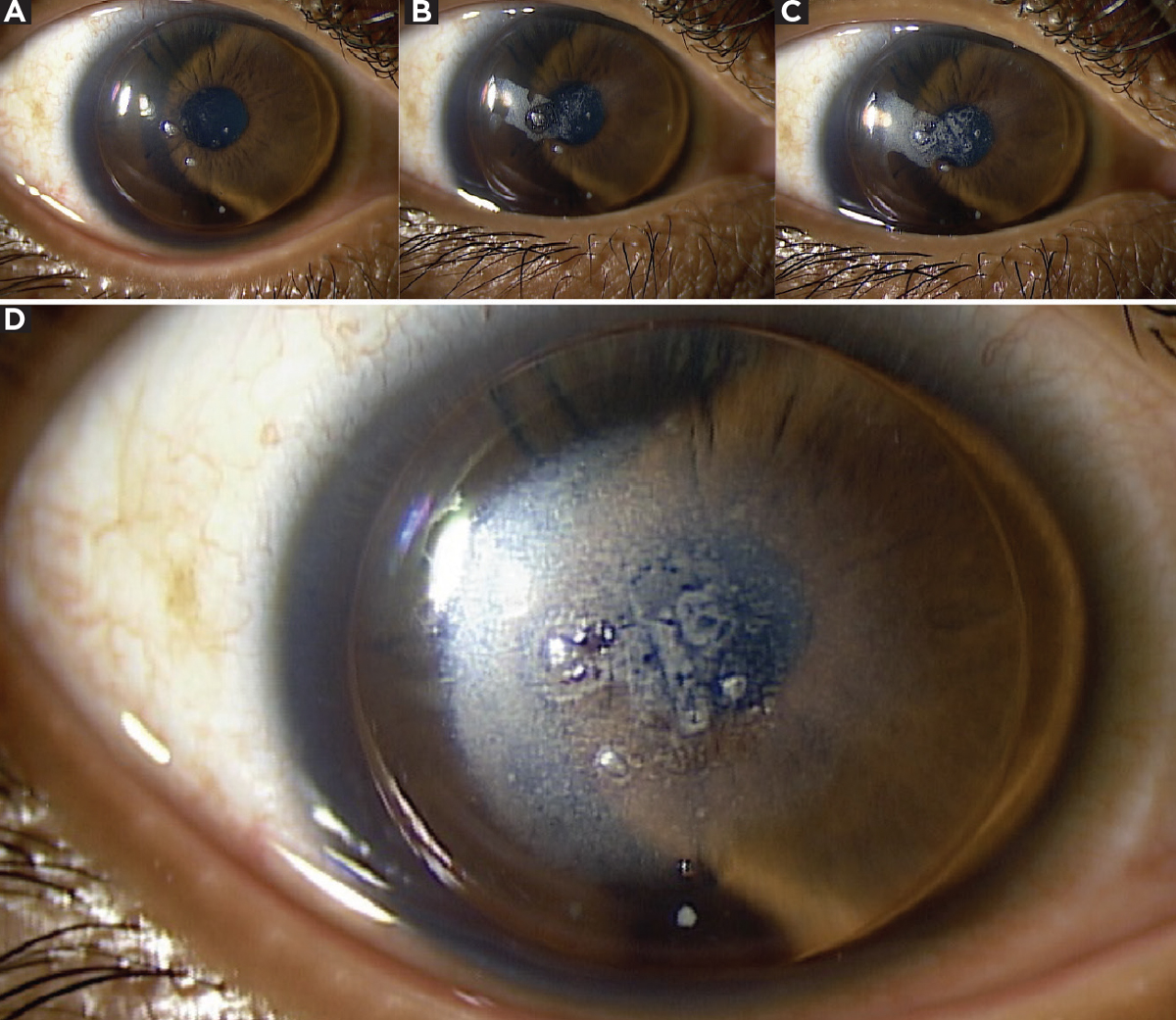
Figs. 2a-d. Time-lapse compilation of photos showing inter-blink non-wetting OD in case two patient. Figure 2a shows lens just after blink with lipid deposits. Photos from moments after that reveal formation of front surface haze (2b and 2c) with full extent of non-wetting visible in 2d. Click image to enlarge. |
Case Two
A 32-year-old male presented with long-standing blurry vision OU but denied any changes since his last exam. He says he sees well with his habitual pair of 18-month-old GP corneal lenses and reported using Boston Advance Comfort, but not on a daily basis. He denies the use of any conditioning or soaking solutions. He admits to sleeping in his lenses nightly and essentially wearing them 24 hours a day. He only removes the lenses when his eyes are irritated, at which time he cleans them with Boston Advance Cleaner, rinses with water and reapplies them.
He denies any comfort or vision issues at this time. The last eye examination was 18 months prior where he was noted to have myopic degeneration. He was unsure of his last medical exam but denies having any systemic conditions. He has a history of lattice degeneration. He has no allergies and is not taking any medications.
Entering VA was OD 20/70 (pinhole 20/50) and OS 20/50 (no improvement with pinhole). The patient’s habitual GP lenses are OD 7.67/9.0/-17.75DS and OS 7.65/9.0/-14.50DS corneal lenses in Boston XO2. The fit was lid-attached OU. The fluorescein pattern showed mild central pooling and adequate mid-peripheral bearing in each eye with good centration and movement. The patient accepted an over-refraction of -0.75DS in each eye which improved vision to 20/40 OD, OS. We confirmed that he could reach the expected BCVA of 20/25 in each eye with contact lenses through the application of a clean diagnostic lens with the appropriate base curve.
Each corneal lens demonstrated heavy lipid and protein deposition in several areas across the front surface (Figure 2). The patient was advised to purchase new lenses at this visit. In an attempt to clean the habitual lenses in-office, we chose the Progent cleaning system (Menicon). The lenses were placed in sodium hypochlorite-potassium bromide mixture for 30 minutes then rinsed with the provided saline. Unfortunately, this did not remove the deposits and the patient’s vision did not improve. An additional attempt was made to clean the lens with Boston Laboratory Lens Cleaner, which also did not yield any improvement to the lens nor the patient’s vision.
 |
|
Fig. 3. Assortment of lens deposits OS found in case two, which were not improved after extensive in-office lens cleaning. Lens replacement was recommended. Click image to enlarge. |
Slit-lamp examination revealed mild vessel encroachment at the limbus nasal and temporal in each eye. There was no fluorescein staining in either eye after lens removal. Today’s refraction was relatively stable to previous visits at OD -19.75DS with VA 20/30 and OS -17.25 -2.50 x 165 with VA 20/25. The dilated fundus evaluation revealed stable white-without-pressure and lattice degeneration OU.
We re-educated the patient on the importance of nightly lens removal and cleaning procedures. He was advised to replace his lenses as the deposits are extensive and were not removed with our in-office cleaning procedures. We also discussed the limitations on the patient’s vision. Though he stated he was happy with his entering acuity, it was reduced to 20/70 in the poorer seeing eye. We also discussed the importance of having backup glasses in order to limit lens wear time.
In both of these cases, the patients will benefit from lens replacement. Particular attention should be given to discussing the benefits of nightly lens removal and cleaning in order to prevent lens deposits from forming on new lenses. Routine lens cleaning allows for effective deposit removal and the protection of lens surface integrity.2 The use of specialized cleaning solutions containing both non-ionic (lipid-specific) and anionic (protein-specific) surfactants prior to lens conditioning will ensure the new lenses stay clear and deposit-free. The addition of a weekly enzymatic cleaner can also help remove additional protein deposits.
Another consideration would be the addition of a polyethylene glycol coating to new lenses to enhance lens wettability; however, this would require a change away from abrasive lens care products and discontinuation of weekly enzymatic cleaner. Interim visits (for example, a six-month follow-up) can also ensure that the patient is staying on track with the proper cleaning procedures, the lenses remain clear, and their anterior segment condition has not deteriorated.
1. Bennett ES, Henry VA. Gas-permeable lens problem solving. Clinical Manual of Contact Lenses. 4th ed. Lippincott Williams & Wilkins, 2014. 2. Boston Materials and Solutions Guide. www.fit-boston.eu/downloads/pdf/ProductGuideEN.pdf. 2011. Accessed April 25, 2022. |


