 |  |
While managing presbyopia can be challenging, many opportunities exist to correct distance and near vision with contact lenses. Presbyopic patients, however, are more likely to develop dry eye and suffer from the resulting discomfort that studies have found is the most common reason for discontinuing lens wear.1,2 To give presbyopic patients a better chance of success with contacts, we must optimize the ocular surface by keeping it as healthy as possible.
As the population continues to age, presbyopia affects more people, yet few presbyopic patients wear contacts. There is a large unmet need that we have the opportunity to rectify. This article summarizes multiple vision correction options for patients with presbyopia. By keeping an open mind and knowing your options, you will be able to optimize your patients’ visual outcomes.
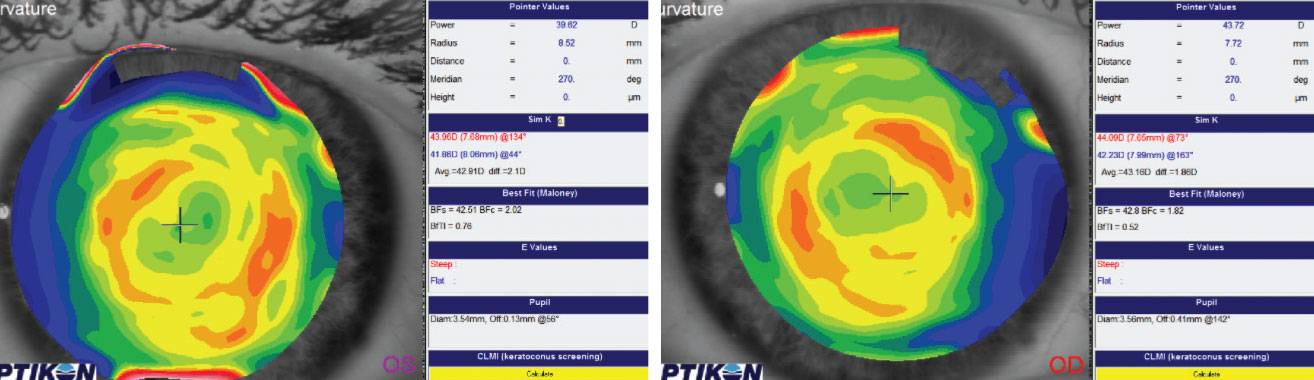 |
| Post ortho-K scans display inferior temporal centration of the treatment zone. |
Multifocal Lenses
These are one of the most frequently discussed vision correction options for presbyopic patients. Multifocal designs are all based on the principle of simultaneous vision, which often requires some degree of adaptation for the best visual outcomes. With simultaneous vision, distance and near optics focus on the retina at the same time to provide binocularity for patients. The differences in the way each multifocal design delivers optics to the eye are often the deciding factors when patients are presented with multiple lens options.
While patients with less than 1.00D of refractive astigmatism are often successful with multifocals, those with more than 1.00D are usually not compensated for appropriately and may notice the uncorrected astigmatism. In these cases, we turn to toric multifocal lenses—customizable specialty lenses.
Even though soft multifocal contact lenses are a top choice for doctors who are fitting presbyopic patients, gas permeable (GP) lenses present another opportunity for vision correction. These lenses are designed to have a smaller diameter than the horizontal visible iris diameter. The distance optics are usually in the center and progress to near optics in the periphery of the optical zone. When the lenses are aligned appropriately over a patient’s visual axis, most of the optical zone will be devoted to the patient’s distance optics. As the patient moves their eyes down to look at something in close proximity, the lens shifts so the patient is able to look through a portion of the lens devoted to the near optics.
If a patient’s corneal astigmatism is similar to their refractive astigmatism, it is usually corrected with a spherical lens through the tear film created between the posterior surface of the GP lens and the cornea. If the astigmatism increases, there is a greater chance of lens flexure, which could potentially cause residual astigmatism to manifest. In this case, the lens may either need a back surface toric or a bitoric design. Fortunately, these designs can be incorporated into multifocal lenses.
An alternate option available in a GP is a segmented bifocal. In this design, the distance optics are located in the superior portion of the lens, and the inferior portion of the lens contains the near optics. There is a definitive separation between the superior and inferior portions of the lens. In order to stabilize the lens, it can be truncated, prism ballasted or both. The best vision is achieved when there is appropriate centration while viewing through the distance portion and appropriate translation while viewing through the near portion. Therefore, having an appropriate inferior lid position is critical.
Monovision
While not as widely discussed as other treatment options, monovision provides vision correction opportunities for presbyopic patients who are unable to adapt to multifocal lenses but are still interested in continuing or initiating lens wear. Monovision corrects dominant eyes for best-corrected distance vision and non-dominant eyes for best-corrected near vision. Each monovision patient is able to view distant objects with their dominant eye and near objects with their non-dominant eye.
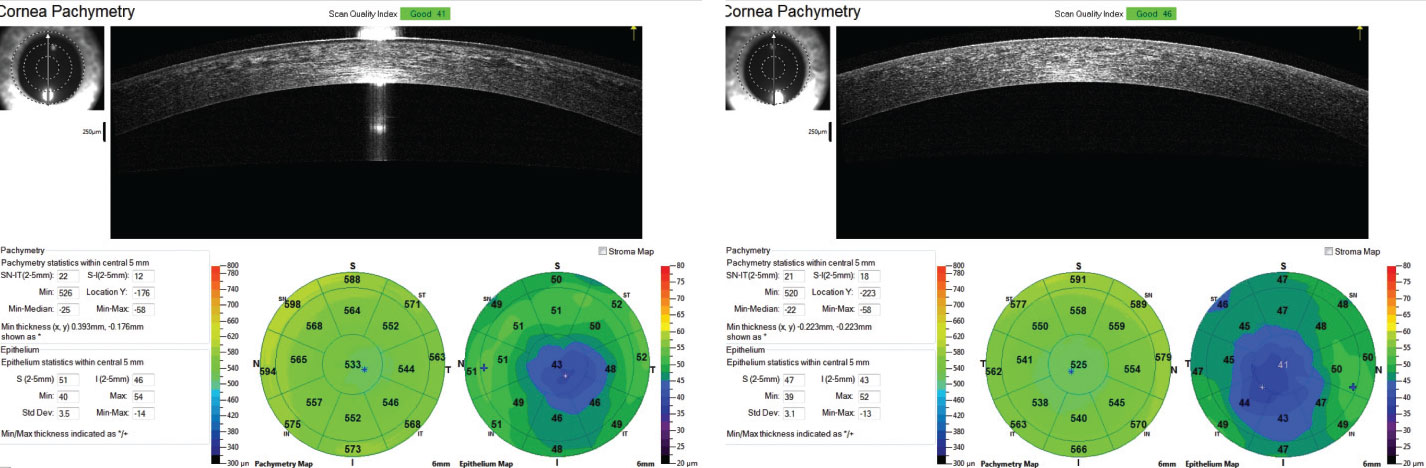 |
| Corneal and epithelial thickness mapping shows inferior temporal thinning consistent with a decentered treatment zone after treatment. |
Ortho-K
With a longstanding record of success, ortho-K is an important treatment option for myopia management, provides a viable option for patients interested in alternate ways to treat their refractive error and mitigates symptoms of lens-induced dry eye. This procedure, however, is often overlooked when correcting myopia and astigmatism.
Appropriate centration of the treatment zone is critical in obtaining the best visual results. Post-treatment topography and OCT measurements of the cornea provide valuable data about the centration of the treatment zone and whether the fit needs to be altered to optimize centration.
There is a significant reverse geometry curve created outside the pupil border that provides the early presbyopic patient some level of low add power. To picture this, consider a lens with its distance optics in the center and its near optics in the periphery. Modifying the treatment zone by making it smaller in the non-dominant eye can also add additional plus power. For situations in which there is not enough plus power delivered to the eye, monovision may be the way to go.
Hybrid Lenses
This unique design presents another option for presbyopic patients and combine the characteristics of a GP and a soft lens—the center of the lens is a GP, and the peripheral portion is a soft lens. The GP part delivers the prescription and appropriate fit characteristics. When refractive astigmatism is similar to corneal astigmatism and is present in a low to moderate amount, the GP center can correct the astigmatism. The soft skirt of the lens provides similar stability and comfort to a soft lens, which requires less adaptation time than a GP.
Scleral Lenses
Usually reserved for fitting corneal abnormalities (e.g., ectasia, irregular surfaces, severely compromised corneas), scleral lenses are also available to presbyopic patients. When fit appropriately, these lenses should rest on the conjunctiva and underlying sclera and vault over the cornea and limbus. Those who are unsuccessful with scleral multifocal designs should consider monovision. Overall, scleral lenses allow patients to experience remarkable improvements to their sight and can minimize the need for glasses.
When working with presbyopic patients, we must maximize their functionality and minimize their need for glasses. Because we cannot promise we will be able to eliminate glasses use entirely, it is important to set realistic expectations before beginning the fitting process. Our presbyopic patients are bound to have success with at least one of the numerous vision correction options available to them. Our job then is to help each patient find the best fit for them.
1. Dumbleton K, Woods CA, Jones LW, et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Cont Lens. 2013;39(1):93-9. 2. Chalmers RL, Hunt C, Hickson-Curran S, et al. Struggle with hydrogel contact lens wear increases with age in young adults. Cont Lens Anterior Eye. 2009;32(3):113-9. |


