The focus on myopia management in children has expanded tremendously over the past 10 years. In 2010, there were nearly two billion people—28.3% of the world’s population—with myopia, yet at that time, treatment for myopic progression was rarely employed.1
In North America alone, a growth rate of 6.2% was observed between 2000 (28.3%) and 2010 (34.5%). The prevalence of myopia in this region is expected to further rise to a whopping 58.4% by 2050. Worldwide projections are at 49.8% for 2050, which means an estimated five billion people globally will be myopic and one billion will have high, or pathologic, myopia by that point.1
The consequences of high myopia extend beyond the standard burden of health care and workplace opportunity costs associated with low and moderate myopia, and include retinal detachment, glaucoma, cataracts, amblyopia, maculopathy and choroidal neovascularization.2-4 In 2010, some 277 million people in the world (4%) were pathologically myopic, up from 163 million (2.7%) in 2000, with this number expected to rise to one billion people by 2050.1 Needless to say, in 2020, the concerning magnitude of increasing myopic prevalence in children is fully realized, and eye care practitioners are increasingly prescribing interventions to reduce the rate of myopic progression.5
Genetics, environment, behavior and visual feedback are among the many factors associated with the risk of myopia development and progression. The strategies used in myopia management commonly target the most modifiable of these factors, such as visual feedback. The important role of the retinal image during myopia development is evidenced by years of animal models showing that peripheral hyperopic defocus is a stimulus for eye growth, and that myopic defocus stimulates a reduction in growth.6 The retinal image focus in the central and peripheral retina has been found to be modifiable using different refractive techniques, and as such, the strategies for myopia management are predominated by refractive treatments.
Among the most effective and practical myopia control treatments currently available are contact lenses, with both orthokeratology and soft multifocal lenses aiming to create peripheral myopic defocus and presumably reduce the optical signal for eye growth.
The Bifocal Lenses in Nearsighted Kids (BLINK) study was completed in late 2019 and recently published in the Journal of the American Medical Association (JAMA). This study was the largest prospective randomized clinical trial to evaluate the efficacy of soft multifocal contact lens design in the management of myopic progression in children. This article summarizes and unpacks the study’s findings and uses them as a guide toward practicing evidence-based clinical management of childhood myopia.
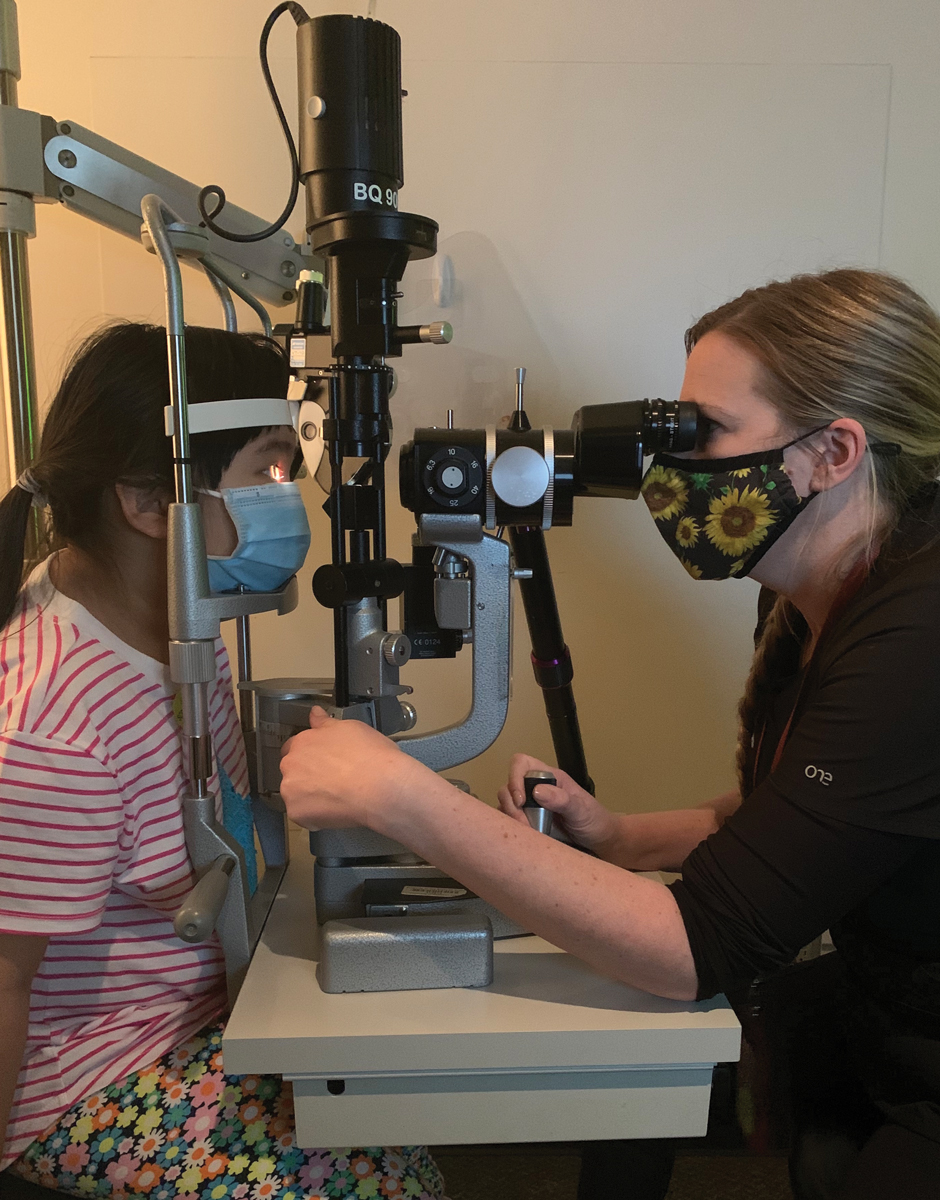 |
BLINK validated an approach to myopia management using center-distance multifocal contact lenses, which slowed myopia progression by about a half-diopter over three years. Subjects were highly motivated; hence, the study’s 97.6% retention rate. Click image to enlarge. |
The BLINK Study
Doctors looking for clarity on the role of multifocal contact lens effects on myopia will find much to appreciate in this clinical trial.
Study design. The BLINK study was a three-year clinical trial that recruited 294 children from the Ohio State University and the University of Houston and fit them in spherical or bifocal soft contact lenses. The subjects were between the ages of seven and 11 with less than 5D of myopia and less than 1D of cylinder (i.e., school-aged myopes without any signs of pathological myopia).
Over the course of the study period, subjects wore the contact lenses daily and underwent yearly comprehensive examinations that included refractive error, axial length, peripheral refractive error and axial length, accommodative lag and choroidal thickness measurements. Subjects were monitored closely for compliance and adverse events. Of the total subjects recruited, 287 completed the study. This extremely high retention rate is not only a testament to the tenacity of the investigators, but also to the motivation of families to receive this type of myopia management.
The contact lenses chosen for the study group were center-distance multifocal contact lenses with either a +1.50D add or a +2.50D add (Biofinity “D” multifocal lenses, CooperVision). A spherical design was picked for the controls (Biofinity spherical lenses, CooperVision). These commercially available lenses were selected because the center-distance and mid-peripheral add designs lend nicely to the myopia management optic needed to create peripheral myopic defocus in the retina. The two different-powered bifocal designs were selected to evaluate a potential dose-dependent effect, which would be seen if the +2.50D add provided a greater reduction in myopic progression than the +1.50D add.
The study participants were split equally between the three groups to wear either the single vision, +1.50D or +2.50D lenses. Lens powers for the subjects were selected based on the spherical equivalent manifest refraction. It should be noted that, on average, an additional -0.50D was incorporated into the sphere power of the lenses (beyond the predicted power based on the spherical equivalent after vertexing) to provide adequate vision.
Outcomes. The ultimate purpose of BLINK was to evaluate the effectiveness of these center-distance soft multifocal lens designs on slowing progression of myopia in children, and the primary outcome was the three-year change in spherical equivalent cycloplegic autorefraction as measured by an open-field autorefractor (Grand Seiko).
The results showed that subjects in the high add treatment group progressed by -0.56D (95% CI: -0.70D to -0.41D) over three years, those in the medium add group progressed by -0.85D (95% CI: -0.99D to -0.70D) and those in the control group progressed by -1.01D (95% CI: -1.15D to -0.87D) over three years, which was -0.45D more than the high add treatment group. This signified a statistically and clinically significant treatment effect in the high add group, providing evidence that high add center-distance multifocal soft contact lenses are effective in reducing myopic progression in children.
As expected, axial length also increased the most in the control group (0.62mm; 95% CI: 0.56mm to 0.69mm) and the least in the high add group (0.39mm; 95% CI: 0.32mm to 0.46mm), with the medium add group falling in the middle (0.55mm; 95% CI: 0.49mm to 0.62mm). Again, these findings confirm the efficacy of the treatment in the high add group, which experienced less axial length growth than the control group by an average of 0.23mm over the three-year test period. These findings are comparable with the results of the MiSight three-year randomized clinical trial (0.32mm less axial elongation than the control group).7
In addition to measuring the efficacy of soft contact lens treatment for myopic progression, the BLINK study also collected data on adverse events in this pediatric population. These side effects will be more thoroughly assessed in a follow-up paper, but initial reports show that no serious adverse events occurred in the children in this study. Those that did occur were typically mild and included giant papillary conjunctivitis, infiltrative keratitis and ocular allergies.
BLINK study subjects were as young as seven years old and were not at a greater risk for contact lens complications than their older peers. Other studies, such as the Contact Lens Assessment in Youth (CLAY) study, have confirmed that the risk of serious adverse events is low with soft contact lens use in children.8-10 However, it’s worth emphasizing that many of the complications in these studies occur due to allergies, solution sensitivities and poor cleaning, which suggests that they could be reduced with the use of a daily disposable lens modality rather than the monthly lens used here. With the increasing availability of daily disposable multifocal lens options, it is perfectly reasonable to recommend daily disposable multifocal lenses when available. This could potentially reduce the mild, yet somewhat limiting, complications observed in this study.
The visual data collected from the BLINK study is also quite reassuring, as vision was optimal with the bifocal lenses, with subjects maintaining better than 20/20 vision in high-contrast visual acuity in both the treatment and control groups. Statistically, there was a slight reduction (two letters) in low-contrast acuity with the high add lenses compared with the controls, but this was not a clinically meaningful difference. These acuity findings should assuage some hesitant clinicians’ fears that multifocal contact lens treatment may affect visual performance in the developmental years of a patient’s life; the study’s findings suggest that these kids are able to achieve visual success with these lenses.
Translating the Data into the Clinic
The primary clinical relevance of this study was to show that center-distance multifocal lenses can reduce the refractive progression and axial elongation in myopic children. This study strengthens the evidence for multifocal lens use and specifically recommends higher add powers (like the +2.50D add used here) for the maximum effect of the lenses to take hold.
Key clinical take-aways. Establishing a scientifically sound relationship is an important first step in curtailing myopia’s advance. Translating science to practice is the next step. Consider the following:
1) Multifocal contact lenses work to slow myopic progression, and the response is dose-dependent.
Higher adds should be recommended whenever possible. Keep in mind that higher add powers may require a greater amount of minus in the spherical power. We’ve found that approximately -0.50D added to the vertexed manifest power for a +2.50D add lens is necessary to achieve adequate vision. Clinicians need not be hesitant to add this power if it improves vision, as we have shown that even with this added minus power, treatment is efficacious and vision is adequate at distance and near.
The BLINK study and others have not yet evaluated the optimal amount of add power for maximum myopic management; it could be different for different eyes which have different prolate profiles.11
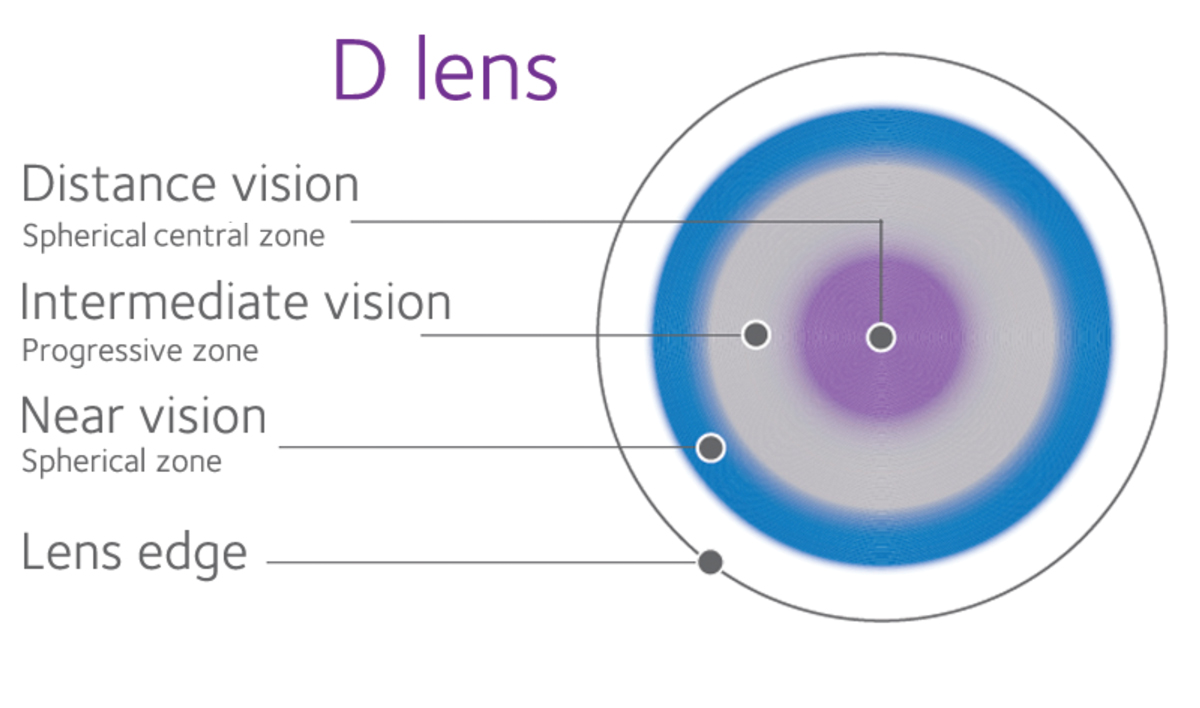 |
Schematic of the Biofinity “D” multifocal contact lens. Click image to enlarge. Image source: CooperVision |
2) Age and severity play a role.
The BLINK study and others that have proven the efficacy of multifocal contact lenses have primarily included children with relatively low levels of myopia. While the studies show promising results in these children, those with pathologic myopia at onset (i.e., >6D), those who develop myopia at a very young age (i.e., <5 years) and those with other predisposing risk factors should be counseled accordingly.
Be upfront with patients and their families about a potentially more severe diagnosis and the lack of clear evidence regarding their treatment options. Set appropriate expectations moving forward. More studies are needed in high-risk and high myopic groups to determine the outcomes of different myopia management approaches in these patient populations.
3) Thoroughly educate patients and their parents.
We have work to do to increase public health awareness of myopia, but until then, it must be done thoroughly in the office. Educating patients and their parents on expectations for vision, treatment and adverse events is critical to success:
• Patients should be able to achieve good vision with the lenses. The BLINK study and others have shown that visual acuity at distance and at near are both comparable with single vision contact lenses. However, as we can see with presbyopic patients, some visual systems respond better to multifocal optics than others. It would be prudent to expect that about 5% to 10% of patients will struggle with subjective visual success in multifocal lenses, either due to the multifocal or uncorrected astigmatism. These patients may require a multifocal toric or another customized lens for success.
• Treatment for myopia is not able to halt progression. A 40% to 50% reduction in myopic progression is an appropriate goal, but this can be tricky to track on an individual basis. An optimistic goal is to aim for 0.15mm or less change per year in axial elongation, which would approximately line up with the average progression seen in the highest treatment group of the BLINK study. Realistic expectations, however, are vastly variable and depend on risk factors such as previous progression, level of myopia and age.
• Serious complications are rare, but specific education on compliance and contact lens care is obligatory. Children are a vulnerable population and must be followed carefully for the best outcomes.
Well-positioned for the Future
The conclusions the BLINK study arrived at can help practitioners feel more confident when recommending commercially available multifocal contact lenses for myopia management in children, especially seeing as high add multifocal contact lenses are a safe and effective strategy for reducing myopic progression in school-aged children.
The study has moved into the BLINK 2 phase, in which all subjects will wear the +2.50D add for the next two years and then single vision lenses for the final year of the study. Stay tuned, as this important study continues to provide information on how to best manage our children with contact lenses to reduce myopic progression.
Dr. Walker, a NECO 2013 grad, is currently part-time faculty at the University of Houston College of Optometry while also completing her PhD, studying the effects of scleral lenses on the ocular surface.
1. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. 2. Smith T, Frisk K, Holden B, Fricke T, Naidoo K. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ 2009;87:431–7. 3. Fricke TR, Holden B a, Wilson D a, Schlenther G, Naidoo KS, Resnikoff S, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ 2012;90:728–38. 4. Ikuno Y. Overview of the complications of high myopia. Retina 2017;37:2347–51. 5. Dolgin E. The myopia boom. Nature 2015;519:276–8. 6. Smith EL, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res 2009;49:2386–92. 7. Chamberlain P, Peixoto-De-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci 2019;96:556–67. 8. Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci 2017;94:638–46. 9. Lam DY, Kinoshita BT, Jansen ME, Mitchell GL, Chalmers RL, McMahon TT, et al. Contact lens assessment in youth: Methods and baseline findings. Optom Vis Sci 2011;88:708–15. 10. Sorbara L, Zimmerman AB, Lynn Mitchell G, Richdale K, Lam DY, Kinoshita BT, et al. Multicenter testing of a risk assessment survey for soft contact lens wearers with adverse events: A contact lens assessment in youth study. Eye Contact Lens 2018;44:21–8. 11. Matsumura S, Kuo AN, Saw SM. An Update of Eye Shape and Myopia. Eye Contact Lens 2019;45:279–85. |


