 |
A 51-year-old white female presented after a week of right eye tenderness, especially upon eye movement. The nasal quadrant appeared hyperemic and slightly edematous and did not fully blanch with 2.5% phenylephrine. Her intraocular exam was unremarkable. She was diagnosed with mild scleritis and conservatively started on 800mg ibuprofen and topical 1% prednisolone acetate four times a day.
Scleritis is an inflammatory process that involves dilation of the superficial and deep episcleral vessels, resulting in a bluish-red hue and the sclera becoming edematous and painful. The patient may complain of tearing, blurred vision and photophobia.
Scleritis is classified in several ways: anterior or posterior, nodular or diffuse, necrotizing or non-necrotizing, and infectious or non-infectious.
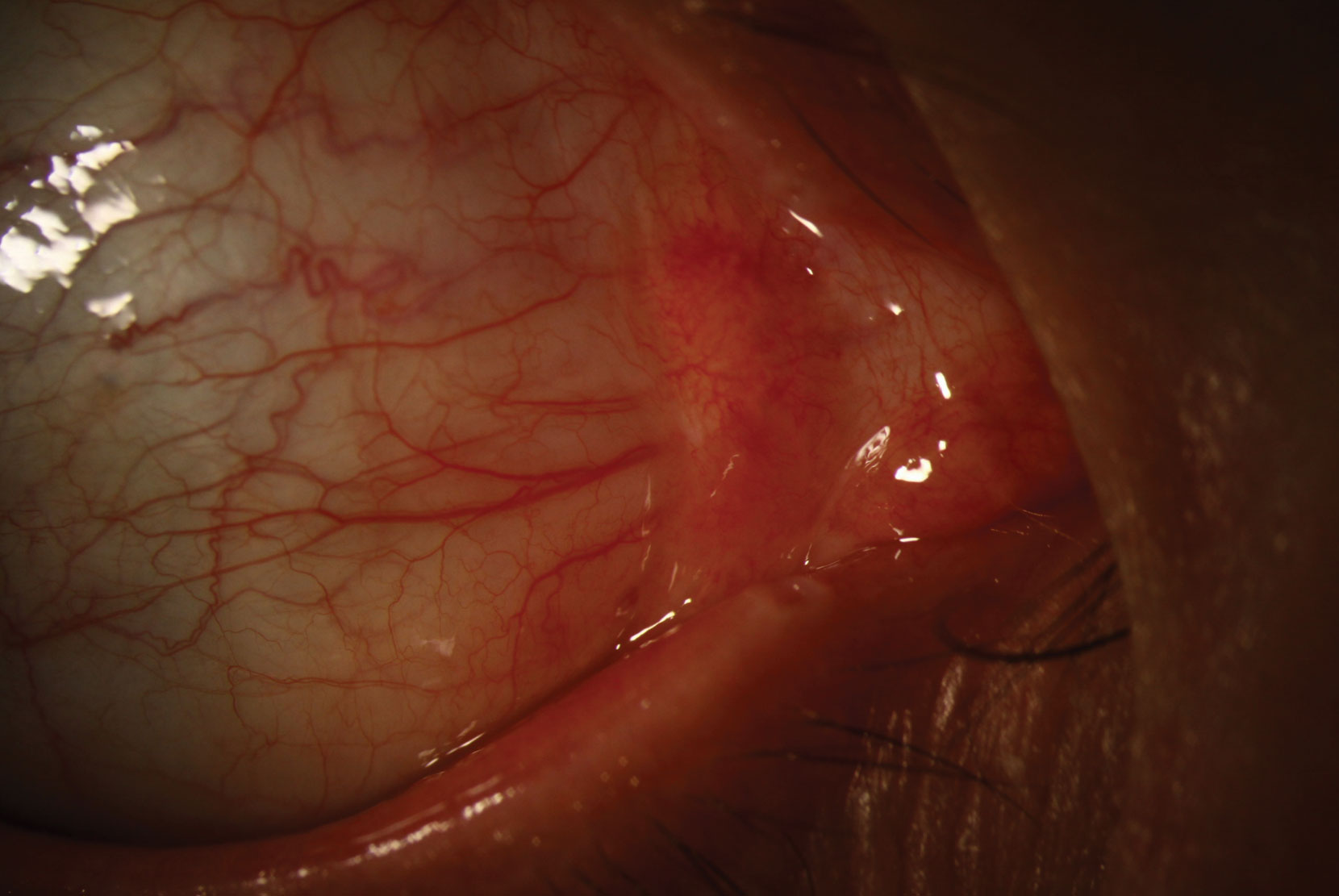 |
| Scleritis is an inflammatory process that involves dilation of the superficial and deep episcleral vessels. Click image to enlarge. |
Anterior, non-necrotizing, non-infectious scleritis is the most common form. In the nodular version, there is visible elevation with engorged scleral vessels. Vision is rarely affected, unless there is concurrent involvement of the cornea or uveal tract. Infection is responsible for about 5% to 10% of cases of anterior scleritis and is typically associated with trauma (89%) or surgery.1,2 Visual prognosis is guarded with infectious scleritis.
Systemic diseases associated with scleritis include rheumatoid arthritis (89% of scleritis), systemic lupus erythematosus, inflammatory bowel disease, sarcoidosis, polyarteritis nodosa, the seronegative spondyloarthopathies and multiple forms of systemic vasculitis.3
The first-line therapy for noninfectious scleritis is oral NSAIDs and prednisone. Topical steroids are useful when there is coexisting intraocular inflammation or mild disease but typically fail if used without systemic medications. Steroid-sparing immunosuppressives, such as methotrexate, are started if the patient cannot be successfully tapered below 10mg of prednisone without symptoms or clinical signs of active scleritis.
| 1. Guerrero-Wooley RL, Peacock JE Jr. Infectious scleritis: what the ID clinician should know. Open Forum Infect Dis. 2018;5(6):ofy140. 2. Hodson KL, Galor A, Karp CL, et al. Epidemiology and visual outcomes in patients with infectious scleritis. Cornea. 2013;32(4):466-72. 3. Akpek EK, Thorne JE, Qazi FA, et al. Evaluation of patients with scleritis for systemic disease. Ophthalmology. 2004;111(3):501-6. |


