What was once one of the more popular methods of mitigating contact lens–related discomfort is now often relegated to an afterthought. Piggyback fitting, which involves placing a soft lens beneath a corneal rigid gas permeable (GP) lens, was once the primary tool practitioners employed to reduce discomfort in those who relied on the vision provided by their rigid lenses.
Previous generations of hydrogel contact lenses failed to provide sufficient oxygen transmissibility and tear exchange to preserve corneal physiology. Newer silicone hydrogel soft lenses, in conjunction with improved rigid GP technology, have rectified many of these concerns.1 With the explosion of scleral lens technology, the art of piggyback fitting is not often discussed. However, it remains a valuable tool that practitioners would be wise to use.2
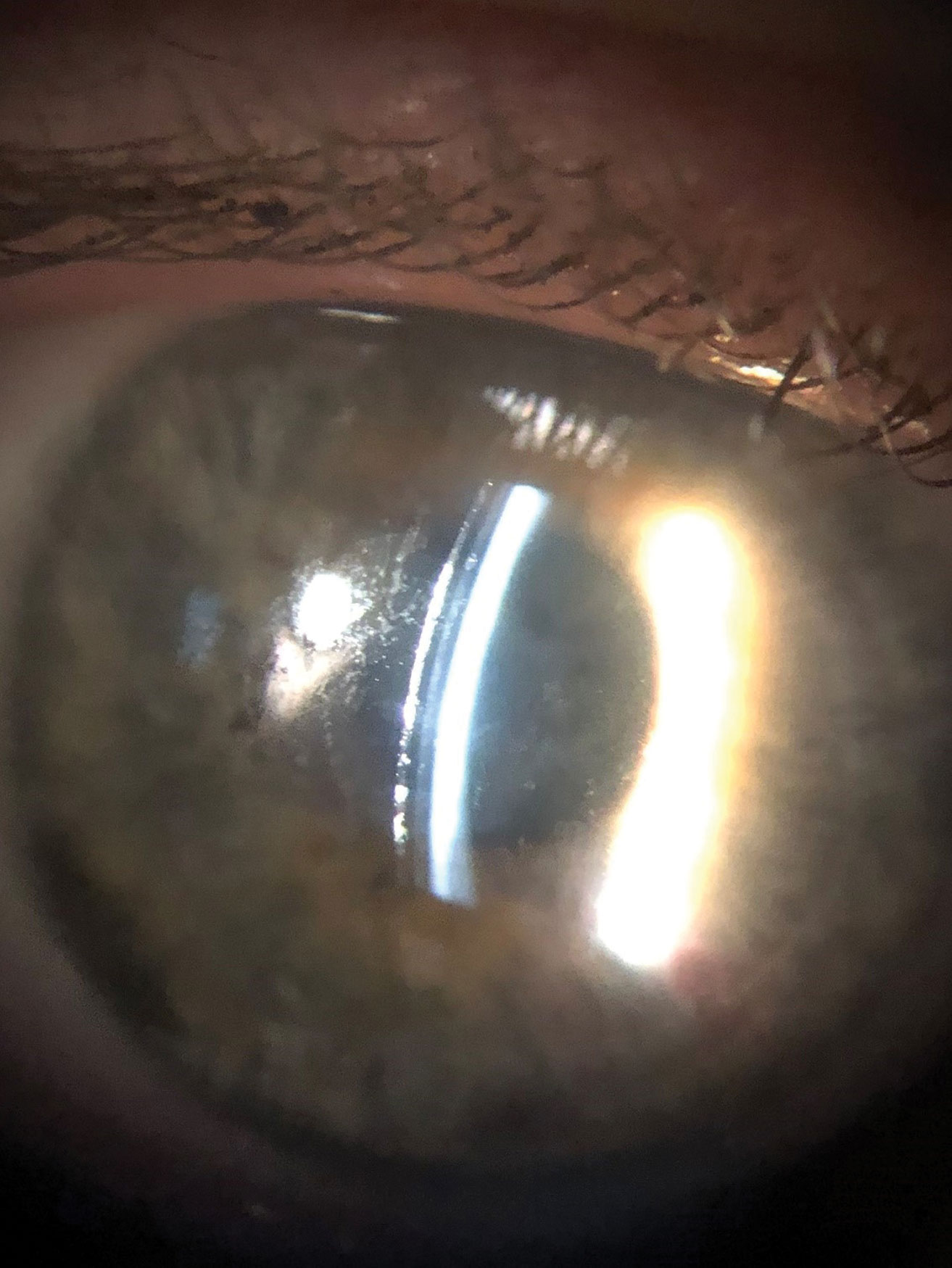 |
| This poorly wetting scleral surface could benefit from adding a soft lens. Click image to enlarge. |
Setting It Up
The beauty of piggyback fitting lies in its simplicity. The practitioner first fits the desired rigid GP lens and achieves the best lens-to-cornea fitting relationship possible. When the corneal GP is ready to be dispensed, the practitioner places the soft lens on the eye prior to inserting the corneal rigid lens. This helps achieve a cushioning effect, whereas the corneal rigid lens is no longer resting directly on the cornea.
The goal of such a fitting relationship is to maintain the optics of the GP lens while improving overall comfort and avoiding corneal insult.3 This is achieved by ensuring that the soft lens portion of the system achieves some movement along with the rigid lens.
The optics of such a system are remarkably simple as well. The soft contact lens only contributes 20% of its listed power to the overall refractive system.4 Thus, if a nominally powered soft lens is used, the power of the soft contact lens can effectively be ignored when calculating the final power of the corneal rigid lens.
Some practitioners will use a moderately high-plus soft lens, such as a +3.00DS lens, if the location of the cone is low. In these instances, the soft lens may contribute a visually significant amount of refractive power into the system and would require neutralization by a corresponding change in the power of the corneal GP lens.
There is some debate surrounding whether it is best to use a nominal-powered soft contact lens vs. a plus-powered contact lens. The flatter front curvature noted with minus-powered and plano lenses may allow for a more appropriate fitting relationship when the steepest portion of the cornea is central or in the mid-periphery.5 The flatter curvature of the soft contact lens provides some degree of normalization, upon which the rigid GP portion sets; in other words, the flatter front curvature of the soft lens may help to offset the steeper, underlying corneal curvature.
If the practitioner is fitting a regular cornea, then the GP can often be ordered empirically by providing the spectacle prescription and keratometry values. Occasionally, the lab may request corneal eccentricity data.
In the case of an irregular cornea, trial lens fitting is necessary to ascertain the best possible fitting relationship. Ordering these lenses is likewise straightforward; the practitioner will be asked to provide the trial lens base curve, power and over-refraction as well as any changes that are indicated. If a piggyback system is used, the laboratory consultant can calculate any changes to the GP power that may be necessary. The practitioner may also simply provide the final lens data requested if they prefers to work out the calculations on their own.
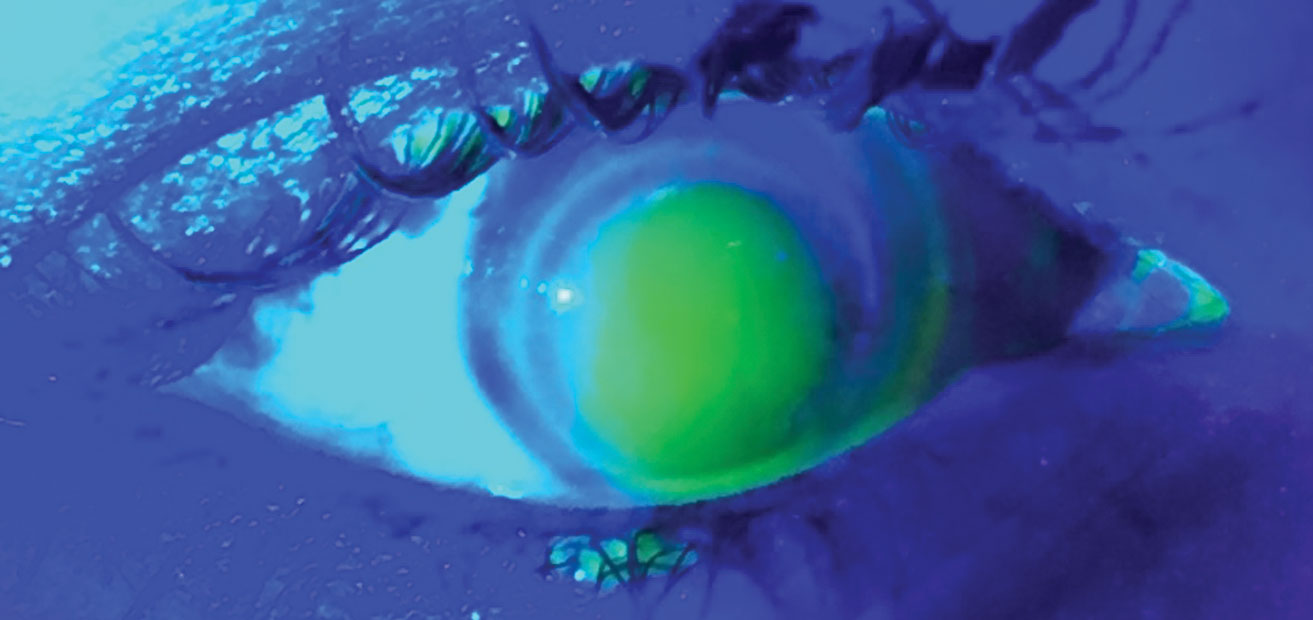 |
| This steep-fitting hybrid lens has a corresponding NaFl pattern. Click image to enlarge. |
Cleaning a Piggyback
One of the drawbacks related to a piggyback system is having the patient maintain different cleaning regimens for each lens. Traditionally, the soft lens would be manufactured from a silicone hydrogel material to promote maximum available oxygen to the corneal structures. In years gone by, this would have uniformly meant that a monthly replacement soft lens was necessary. However, with the increased availability of single use contact lenses, a piggyback system no longer needs be complicated. These daily lenses may also be manufactured in silicone hydrogel materials, thus allowing practitioners and patients alike to benefit from simplicity while maintaining the corneal physiology.
Where Do Sclerals Fit?
Scleral lenses have largely become the favored lenses of practitioners who fit irregular cornea patients. These devices are remarkably customizable and allow visual correction of patients with myriad corneal profiles. The practitioner can achieve comfort by avoiding corneal touch and allowing for the weight of the lens to be borne entirely by the conjunctiva and the underlying sclera. But is there a situation where a piggyback arrangement may be beneficial while also employing sclerals?
In short, using a scleral lens as part of a traditional piggyback system would indeed be rare. Back when base curve alteration was one of the only means possible to adjust sagittal depth, there was some thought that using a soft lens beneath the scleral lens could alleviate mechanical trauma while optimizing the fit in other areas. There are also reports of successful piggyback systems when a soft contact lens is combined with a corneo-scleral lens.6 However, given the array of options available today that allow for extreme customization of an ocular device, the use of a soft contact lens beneath a scleral is no longer in vogue. The physiologic concerns that stem from oxygen availability as well as the cumbersome nature of such a system would steer most practitioners away from such an arrangement.
One niche use of soft contact lenses in conjunction with a scleral lens involves dealing with a poorly wetting scleral lens surface. A non-wetting scleral lens results in a poor visual experience as well as a substandard outcome, since the practitioner is unable to determine a proper refractive endpoint. While you could remove the scleral lens to rehabilitate the surface in a timely manner, this situation is often unwieldy and time-consuming.
Instead, a Dailies Total1 lens (Alcon) may be placed directly on the front surface of the scleral lens. When allowed to sit for 10 to 15 minutes, the lens surface will regain its wettability and the soft lens may be removed due to the unique phospholipid properties inherent in the Dailies Total1 lens. Upon removal of the soft lens, the scleral surface should now wet more appropriately.
Another iteration of a “reverse piggyback” may be beneficial in allowing the patient to “test-drive” a scleral lens while in the office. In a situation where the patient may be hesitant and doubts whether they will be able to appreciate the improved visual performance, place a daily lens mirroring the over-refraction on the front surface of the scleral lens. This would allow the patient to experience true visual potential in a controlled environment. Of course, you may also use a handheld lens to demonstrate to the patient their true visual potential. These uncommon situations may not present on a regular basis, but the available tools may aid the patient and practitioner in achieving a satisfactory result.
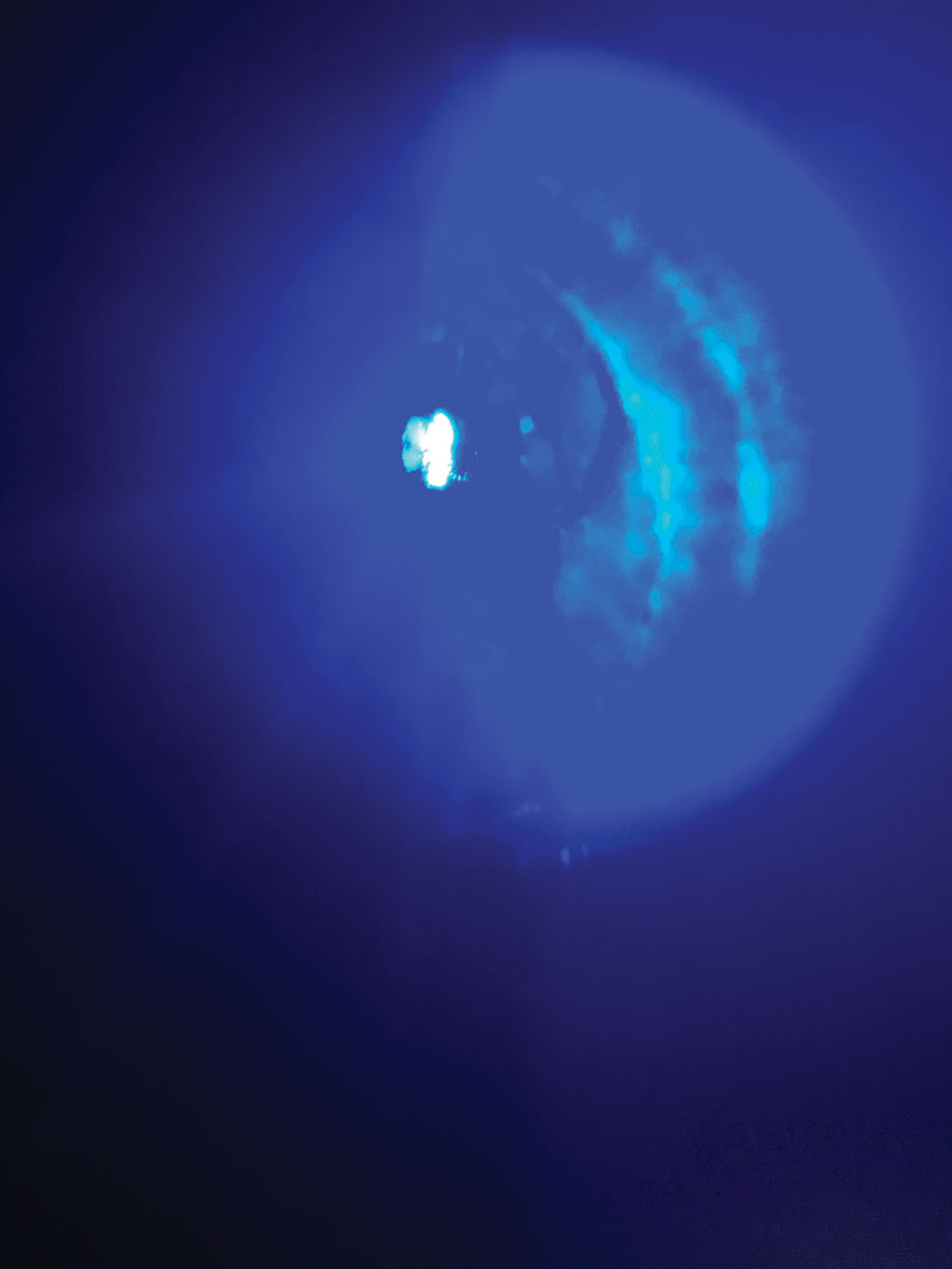 |
| Corneal molding and staining with a tight-fitting hybrid lens. Click image to enlarge. |
History of Hybrids
A more recent option that combines the visual benefits of a rigid GP lens with the improved comfort of a soft contact lens is hybrid contact lenses. First patented in 1977 by Charles E. Erickson and Amar N. Neogi, the first commercially available hybrid lens was launched in 1984 under the trade name Saturn II.7 Due to stresses placed on the soft hydrogel material during manufacturing, this iteration of hybrid lens suffered from the soft skirt tearing as well as corneal adherence and edema.
The original design underwent significant modifications and was re-released under the tradename SoftPerm. While material improvements allowed for an increase in successful fits as compared with the Saturn II lens, issues related to tight lenses, corneal staining and overall discomfort remained a barrier.
A third generation of hybrid lenses received market clearance in 2005. Manufactured and distributed by SynergEyes, four versions of hybrid lenses were initially available. The lenses were marketed as the SynergEyes A (for high astigmatism), SynergEyes KC (keratoconus), SynergEyes PS (post-surgical) and SynergEyes MF (multifocal). The lenses consisted of a GP portion with a dK value of 100 and a HEMA skirt with a dK value of approximately 17.
Due to improvements in manufacturing technology, separation of the skirt from the GP portion became nearly impossible. However, the lenses still exhibited tight-fitting characteristics. Such complications often included corneal staining, corneal molding and lens awareness.
Striving for Corneal Comfort
It was not until the fourth generation of hybrid contact lens technology that significant patient comfort was achieved. With the introduction of the Duette family of lenses (for normal corneas) and the UltraHealth family (for irregular corneas), it was finally possible to provide maximal oxygen availability while maintaining proper corneal physiology. Both the Duette and UltraHealth consist of a hyper-dK rigid GP portion with a measured dK value of 130. The soft skirt is manufactured from a silicone hydrogel material with a dK value of 85.
With the transition away from HEMA materials, the overall fitting characteristics of the lens also required modification. With earlier versions of hybrid lenses, the HEMA skirt possessed sufficient strength to raise the overall clearance of the lens by altering the skirt profile. Silicone hydrogel skirts, however, do not possess this characteristic.8
Practitioners who had become accustomed to steepening the skirt profile to elevate the hybrid lens were now instructed to choose a lens with an overall deeper sagittal depth. The sole role of the soft skirt was to improve centration of the lens. This resulted in far fewer adjustments of the soft skirt profile when compared with the fitting philosophies employed with earlier hybrid lens iterations.
Practitioners may order the Duette family of lenses empirically by providing a member of the SynergEyes consultation team keratometry values, the spectacle prescription and the horizontal visible iris diameter (if available). A calculator is also available on the company’s website if the practitioner prefers to order the lens virtually (synergeyes.com/professional/duette/fitting-calculator/).
If a multifocal lens is desired, the patient’s spectacle add power and pupil size are also necessary. Duette Progressive lenses are available in both center-distance and center-near designs. The center-distance version allows for alteration of the center zone with a target size of 1mm smaller than the pupil diameter in normal lighting. The center-near design has a fixed 3mm zone size.
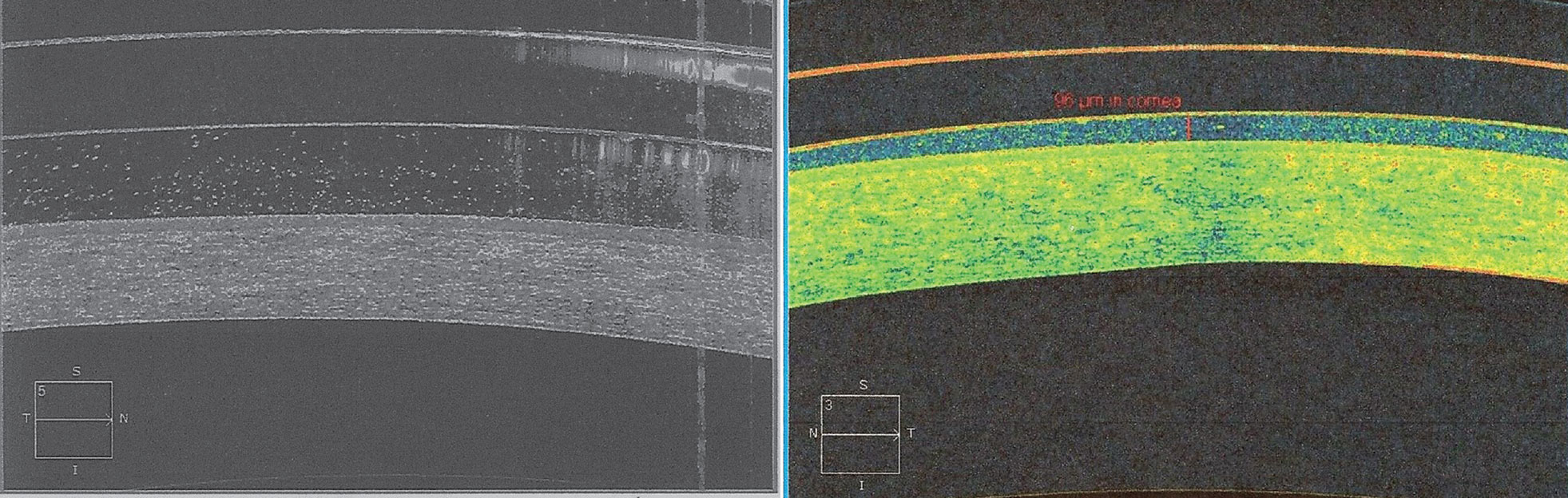 |
| At left, OCT imaging of a scleral contact lens shows debris in the post-lens tear layer. Refitting this patient into a hybrid contact lens resulted in much less debris in the post-lens tear layer. Click image to enlarge. |
Options For The Irregular Cornea
Much like its Duette counterpart, the UltraHealth lens comes in two iterations. The traditional UltraHealth design is typically used for ectatic corneas, such as those traditionally seen in keratoconus. Compared with earlier designs for irregular corneas, this UltraHealth lens has a mild reverse-geometry profile, a more forgiving landing zone and improved oxygen transmissibility.
For corneas that exhibit a more extreme oblate profile, the UltraHealth FC lens has expanded capabilities. The UltraHealth FC is most often used for corneas that have suffered post-refractive surgery ectasia, although it may also have clinical utility for corneas which exhibit an exceptionally low cone.9
Take special care when fitting a patient who has previously undergone radial keratotomy surgery. As the corneal rigidity has been compromised in these cases, these corneas exhibit a propensity to mold to the shape of the lens.10 This may result in prolonged periods of spectacle blur following removal of the contact lens.
An ill-fitting hybrid lens, especially those that result in a tight-fitting relationship, will result in poor movement and poor tear exchange beneath the lens. This may also result in the formation of neovascularization. It has been postulated that chronic dilation of limbal vessels as the result of tight-fitting contact lenses may exacerbate new vessel formation.
Fogging
One area in which hybrid lenses may prove useful as a problem-solver is related to persistent fogging of the post-lens tear reservoir in scleral lenses. Such fogging often occurs due to excessive clearance over the corneal limbus, asymmetric landing of the scleral lens haptics and stagnation of corneal metabolites due to limited tear exchange beneath a scleral lens.11
In such instances, a hybrid lens may prove beneficial to help clear corneal debris due to lower corneal clearance and improved tear exchange. The smaller overall diameter of the hybrid contact lens may also eliminate the need for toric landing zones that are more commonly seen in scleral lenses that land far from the corneal limbus.
Whether using a piggyback arrangement or a hybrid contact lens, the full-scope practitioner has a wide variety of options available to maximize a patient’s vision. While there are limits to the clinical utility of each, piggyback systems and hybrid lenses allow for a more simplistic approach to fitting. Thoroughly understanding their benefits may help you realize how much of a solution the two can be.
Dr. McKinnis practices at the Cleveland Eye Clinic in Avon, OH. He is a Fellow of the American Academy of Optometry as well as a Fellow of the Scleral Lens Education Society.
Dr. McKinnis is a consultant to SynergEyes.
| 1. López-Alemany A, González-Méijome JM, Almeida JB, et al. Oxygen transmissibility of piggyback systems with conventional soft and silicone hydrogel contact lenses. Cornea. 2006;25(2):214-9. 2. Sengor T, Kurna SA, Özkurt Y. High dK piggyback contact lens system for contact lens-intolerant keratoconus patients. Clin Ophthalmol. 2011;5:331-5. 3. Szczotka LB, Lindsay RG. Contact lens fitting following corneal graft surgery. Clin Exp Optom. 2003;86:244-9. 4. Woo M, Weissman BA. Effective optics of piggyback soft contact lenses. CL Spectrum. 2011;26:50–2. 5. Rimero-Jimenez M, Santodomingo-Rubido J, Flores-Rodríguez P, Gonzálex-Méijome JM. Which soft contact lens power is better for piggyback fitting in keratoconus? Cont Lens Anterior Eye. 2013;36(1):45-8. 6. Porcar E, Montalt JC, España-Gregori E, Peris-Martínez C. Corneo-scleral contact lens in a piggyback system for keratoconus: a case report. Cont Lens Anterior Eye. 2017;40(3):190-4. 7. Maguen E, Martinez M, Rosner IR, et al. The use of Saturn II lenses in keratoconus. CLAO J. 1991;17:41-3. 8. Kirchner JK. Why flat skirts are so important in determining the correct lens for UltraHealth. Synergeyes. synergeyes.com/why-flat-skirts-are-so-important-in-determining-the-correct-lens-for-ultrahealth. Accessed July 27, 2020. 9. Alió JL, Belda JI, Artola A, et al. Contact lens fitting to correct irregular astigmatism after corneal refractive surgery. J Cataract Refract Surg. 2002;28(10):1750-7. 10. Bergmanson JP, Walker MK, Johnson LA. Assessing scleral contact lens satisfaction in a keratoconus population. Optom Vis Sci. 2016;93(8):855-60. 11. Blackburn BJ, Jenkins MW, Rollins AM, Dupps WJ. A review of structural and biomechanical changes in the cornea in aging, disease and photochemical crosslinking. Front Bioeng Biotechnol. 2019;7:66. |


