 |
With the increased availability of quadrant-specific scleral lenses, our ability to fit highly asymmetric eyes continues to improve. The following case highlights a patient with profound corneal astigmatism that extended into his scleral anatomy who found success with a quadrant-specific scleral lens.
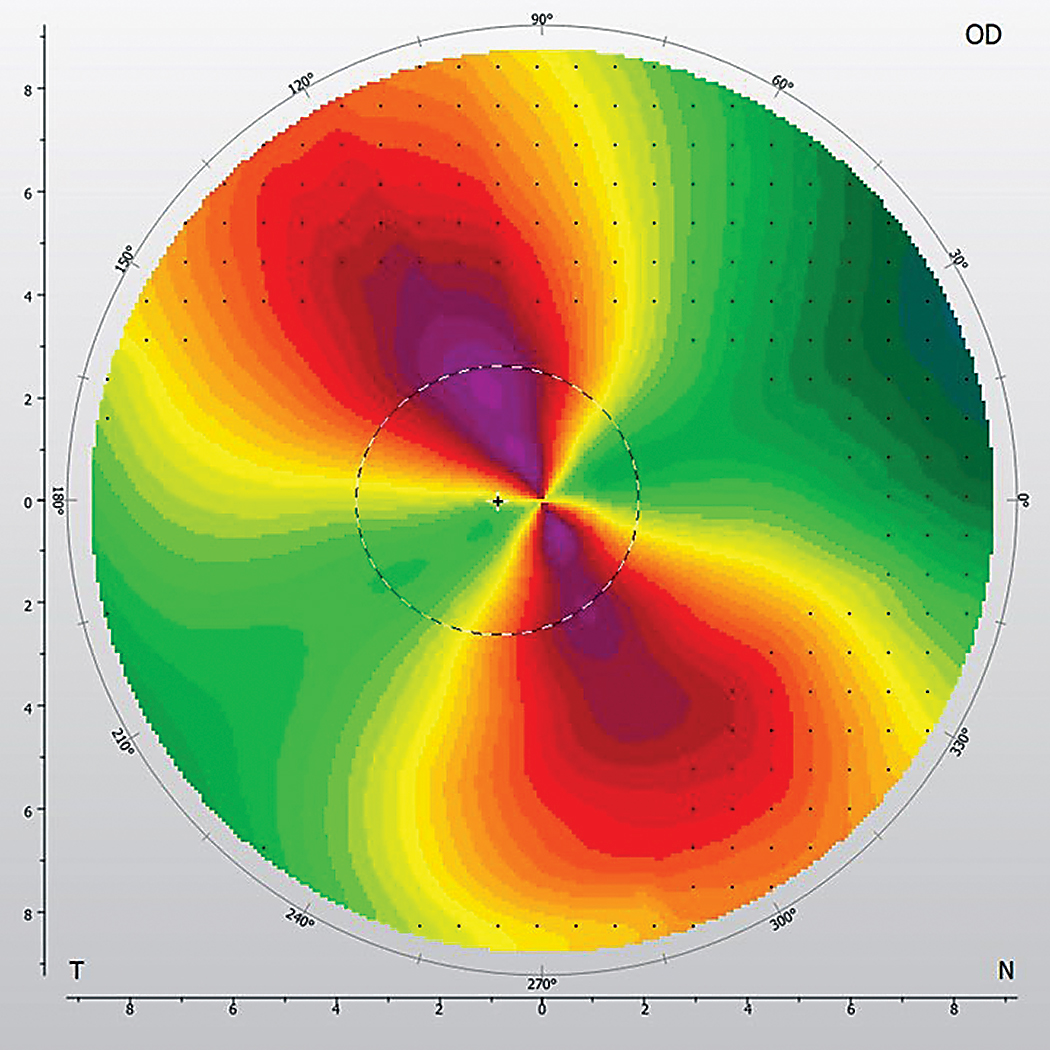 |
Limbus-to-limbus corneal astigmatism. Click image to enlarge. |
The Case
A 47-year-old male presented for a contact lens fitting. He had been wearing glasses since he was a young child; however, he had no history of contact lens wear. He was interested in a contact lens option to wear primarily during exercise. Up until this point, he typically went uncorrected during recreational activities.
Manifest refraction was +1.00 -7.00x037 OD and +0.50 -7.25x157 OS with 20/25 vision OU. Slit lamp exam was not suggestive of ectasia. This was confirmed by topography, which displayed a high degree of oblique but regular astigmatism. The astigmatism was noted as limbus-to-limbus, a generally accepted misnomer that implies the astigmatism extends across the breadth of the cornea based on the pattern extending across the entirety of the topographic image. This contrasts with central corneal astigmatism, in which the astigmatic pattern is confined to the center. It is particularly noteworthy for patients with a high degree of regular astigmatism, as it has been shown that the orientation of the flat corneal and scleral meridians is typically similar in these individuals.1
Based on the patient’s plan to wear contact lenses while exercising, I eliminated corneal GPs from consideration. We ultimately decided on sclerals as an option that would allow for part-time wear, perform well in the intended environment and provide stable vision correction less prone to unacceptable rotation.
Diagnostic Fitting
I used a diagnostic fitting set with a standard 210µm of scleral toricity (Custom Stable Elite lenses by Valley Contax). This is indicated by steps of 30µm with a flat meridian standard of +3 (90µm) and a steep meridian standard of -4 (-120µm).
After 25 minutes of settling, the central clearances in the right and left eyes were 175µm and 150µm, respectively. Limbal clearance was full and appropriate at roughly 25µm. The right lens was rotated 30° to the right, and the left lens was rotated 25° to the left. I judged this rotation by documenting the location of the flat meridian markings (+3) relative to the horizontal meridian.
In assessing the fit of the scleral landing zones, the flat meridians of each eye displayed symmetrical mild edge lift. The superior steep quadrant was aligned, while the inferior steep quadrant displayed excessive edge lift with rapid fluorescein exchange. Even minor manipulation of the eyelid and/or lens allowed air bubbles to rapidly enter the central reservoir of the lens from the inferior quadrant. After a brief evaluation, central bubble formation necessitated the removal and reinsertion of the lenses for further evaluation.
After another period of settling, over-refraction resulted in +2.75 -2.25x035 OD and +2.75 -1.50x145 OS with 20/20 acuity OU. Keratometry over the settled lens yielded a spherical result, confirming no lens flexure was present. As a result, residual cylinder would need to be incorporated as a front toric.
Since the superior and inferior quadrants displayed different fit patterns, a quadrant-specific, rather than a toric, lens design was required. The flat meridian (roughly nasal and temporal in this case) was steepened two steps from +3 to +1. As the superior quadrant was already aligned, it was ordered as standard. The inferior quadrant was steepened by 420µm (-14 steps) to address the inferior edge lift. This was an educated approximation, as the magnitude of edge lift was extreme, limiting precision.
The parameters ordered for quadrants one through four in both eyes were +1, -4, +1 and -18, respectively. To compensate for the rotation present, 30° was subtracted from the over-refraction axis OD and 25° was added OS. The over-refraction, trial lens power (+2.00 OD, +2.00 OS) and trial lens rotation (30° right OD, 25° left OS) resulted in a final power of +4.75-2.25x005 OD and +4.75-1.50x170 OS. When making significant changes in the scleral landing zone, it is possible the ordered lens will not rotate in the same orientation as the diagnostic lens. This may impact the physical and refractive outcomes of the lens. Despite this possibility, a spherocylindrical over-refraction was used to determine the final lens power for this patient.
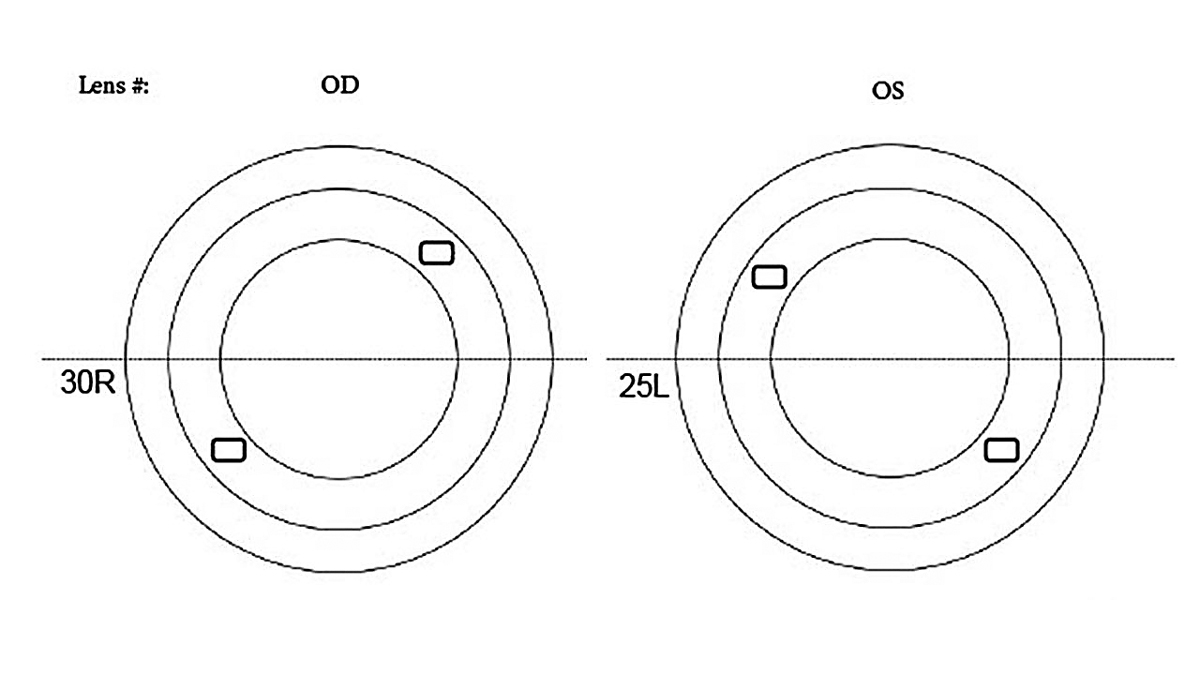 |
| Lens rotation noted during diagnostic fitting. Click image to enlarge. |
Dispensing
After insertion, the lenses were left to settle for 20 minutes. The patient exhibited excellent visual acuity at 20/20 OD and OS, subjective vision improvement, ideal central clearance of 150µm and appropriate limbal clearance. Despite an improved fitting relationship along all meridians, significant edge lift remained in the inferior quadrant of both eyes. An additional 300µm (10 steps) of inferior steepening was incorporated, resulting in -28 steps in quadrant four.
The new lenses were aligned in all quadrants. The patient continued to have excellent vision and noted the lenses as extremely comfortable. The patient enjoyed continual success through the two-year follow-up.
Discussion
Having a comprehensive understanding of scleral shape plays an integral role in a successful scleral lens fitting. Numerous technologies have helped increase our knowledge, including Scheimpflug imaging and AS-OCT. As these imaging techniques become more readily available, we can take advantage of the data we gain from them, even if we do not directly use them in the clinic.
A recent study demonstrated several key findings related to OCT and scleral lens fitting.2 First, corneoscleral and scleral angles of tangency vary circumferentially around the limbus.2 Second, the sclera’s rotational asymmetry generally increases as distance from the limbus increases.2 Clinically, we can generalize that while the sclera is not truly symmetrical even at the corneolimbal transition, its variance is relatively low. Generally, this allows symmetric lens designs to find success when fitting small diameters (≤15mm). At larger diameters, the scleral asymmetry increases to a clinically significant range, indicating the need for asymmetric designs.
The Scleral Shape Study Group extended our understanding of scleral profiles further.3 Reviewing the circumferential elevation profile at 16mm, scleral shape can be grouped into spherical, regular toric, asymmetric single elevation or depression and irregular toric.3 Although these groups do not directly represent specific scleral lens designs, it can be inferred that near this diameter, symmetrical lens designs offer the least utility with toric or even quadrant-specific designs indicated for optimal success in a large proportion of patients. With this information, we can recognize fitting patterns during the fitting process, allowing for more strategic lens designs.
A final point of interest is that scleral shape varies between those with normal corneas and those with corneal ectasia. Those with ectasia are more likely to fall into the latter two, more irregular scleral-shaped groups, suggesting quadrant-specific or freeform lenses (ones aided in design by scleral shape imaging) may be more necessary in this population.4
The patient in this case had one large depression consistent with the asymmetric single elevation or depression group. This necessitated a quadrant-specific design with a final sagittal depth of 870µm from the peak of the flat meridian (+30µm or +1 step) to the trough of the inferior quadrant (-840µm or -28 steps).
This patient’s quadrant-specific lens design was extreme, and I struggled to wrap my mind around his significant inferior scleral depression. I ordered lenses based on what I observed and, after one remake, landed on a pair the patient has been successfully wearing for several years.
I’ve since encountered more cases like this and gained confidence in quadrant-specific designs. Empowered by an understanding of scleral shape patterns, fitters can trust what they see and employ these unique technologies to improve patient outcomes.
1. Macedo-de-Araújo RJ, Amorim-de-Sousa A, Queirós A, et al. Relationship of placido corneal topography data with scleral lens fitting parameters. Cont Lens Anterior Eye. 2019;42(1):20-7. 2. van der Worp E, Graf T, Caroline PJ. Exploring beyond the corneal borders. CL Spectrum. 2010;25(6):26-32. 3. DeNaeyer G, Sanders DR, van der Worp E, et al. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer: the SSSG study. J Cont Lens Res Sci. 2017;1(1):12-22. 4. DeNaeyer G, Sanders DR, Michaud L, et al. Correlation of corneal and scleral topography in cases with ectasias and normal corneas: the SSSG study. J Cont Lens Res Sci. 2019;3(1):e10-20. |


