  |
Corneal vault is a unique property of scleral lenses that can provide distinctive benefits to our patients, particularly those with corneal pathology. This column focuses on troubleshooting corneal health complications induced by the reservoir of scleral lenses and how to approach corneas with difficult pathology.
Causes of Complications
The main corneal health issues induced by the lens reservoir are:
Insufficient vault. This can lead to corneal epithelial disruption, which may cause corneal scarring. Certain conditions, such as Salzmann’s nodules, can be affected in a similar fashion. Insufficient limbal clearance can also result in epithelial disruption, as well as neovascularization and limbal stem cell deficiency (Figure 1).
Lens solutions. Incorrect solution use can lead to toxic reactions with pan-corneal disruptions. Preservatives in the reservoir can cause toxic reactions that mimic punctate erosions or superficial punctate keratitis (Figure 2). Also, problems with lens handling and insertion may lead to reservoir saline spillage and air bubble entrapment, causing localized epithelial desiccation if the bubble is stationary.
Excessive vault. This can be problematic in susceptible corneas, such as those with reduced endothelial function due to conditions like Fuchs’ endothelial dystrophy or corneal transplants like penetrating keratoplasty or Descemet’s stripping automated endothelial keratoplasty. Epithelial bullae, microcystic edema and corneal edema are possible when the cornea cannot manage the physiologic stress induced by a lens.1 Also, excessive vault over the limbal area can lead to conjunctival prolapse, which may adhere to the cornea, leading to vascularized and localized limbal stem cell deficiency.2-4
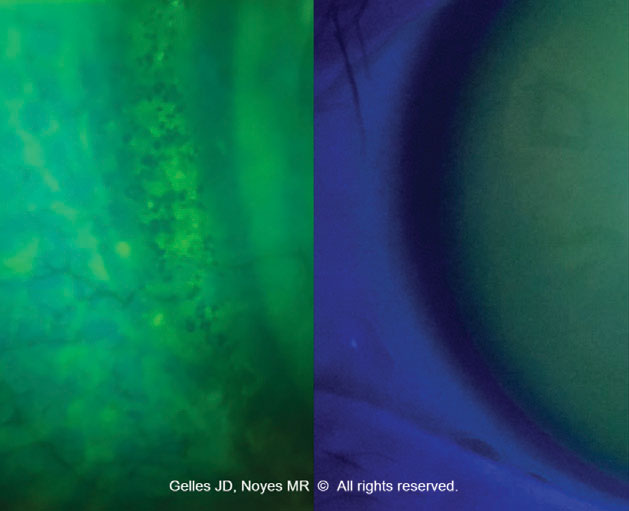 |
| Fig. 1. Epithelial disruption and microcysts due to scleral lens bearing at the limbus. Click image to enlarge. |
Assessment and Identification
A thorough history and vision questioning reveals many of the signs and symptoms of problems with the scleral lens reservoir, though many are non-specific and may arise with other complications. A commonly reported issue is vision clouding with increased wear time, which could indicate a variety of problems related to the reservoir. In corneas with a reduced ability to cope with the induced physiologic stress from the lens, patients may also describe a rainbow around light sources—a Sattler’s veil—indicating corneal edema. Additionally, increasing burning or stinging with lens wear can be indicative of issues in the lens reservoir. Here’s how to evaluate for these issues with the lens on and off:
Lens on. Corneal vault can be assessed in several ways: from slit lamp examination to anterior segment OCT (AS-OCT), or even a-scan ultrasonography. The most common way to distinguish corneal vault is by slit lamp examination. The vault can be assessed using a fine optic section with high-intensity white light illumination. Using known parameters, the corneal clearance can be estimated at the slit lamp. Vault is often easier to assess by instilling a drop of sodium fluorescein in the scleral lens reservoir; however, practitioners should become proficient at clearance evaluation without the use of dye, as patients who are following up do not have it instilled.
Another wau to assess vault is to perform AS-OCT imaging of the lens; this allows for more exact calculation (down to a few microns) and can be particularly useful when corneal pathology must be vaulted. Remember, the ocular surface is a soft, compliant tissue, and initial corneal vault decreases by ~100µm after four hours of lens wear.
Lens off. Evaluate the cornea at the slit lamp with direct white light illumination, specular illumination, sclerotic scatter or retroillumination to reveal subtle pathology (Figure 3). These post-lens removal methods, along with sodium fluorescein and cobalt blue illumination to detect negative and positive staining, aid in finding corneal sequelae of scleral wear, such as corneal touch, toxic reactions, corneal bullae and microcystic edema. Also, tomography can be extremely helpful in monitoring changes to global corneal pachymetry to evaluate induced corneal edema. Ensure sodium fluorescein is not instilled prior to Scheimpflug camera-based tomography, as it may affect the scan accuracy.
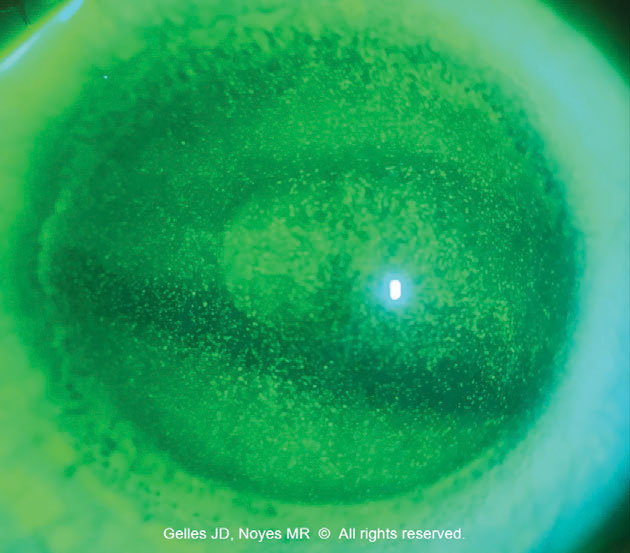 |
| Fig. 2. Toxic keratopathy due to soft lens solution in the scleral reservoir. Click image to enlarge. |
Problem-Solving
There are several ways to counteract issues arising from scleral lens wear:
Lens solutions. A major cause of corneal issues is the incorrect use of solutions. At every visit, confirm the patient’s cleaning regimen. A commonly seen issue is confusion about filling solutions. Prescribe—don’t recommend—lens solutions, and make it clear that they are not to be changed unless directed by you. Patients often confuse or replace solutions based on outside recommendations. Encourage them to communicate changes that have been suggested prior to making them. This prevents complications and builds trust in your expertise.
Another common issue is the use of preserved artificial tears and salines, and even multipurpose lens solutions, as an application fluid. Adopting a simple solution list for patients can be helpful, as an overwhelming amount of information is given during application and removal training.
Clearance. Manage insufficient or excessive lens clearance by changing the sagittal depth in the reservoir or adjusting the base curve to allow for changes in the optic zone or secondary curves in the case of a peripheral cornea and limbus. Some designs allow for independent changes to each region, while with others, a change in one zone affects another.3
For uneven clearance with insufficient corneal clearance in the superior cornea, achieve an even clearance by adding more custom landing zones, such as toric or quadrant-specific haptics, to center the lens.3
Estimates of the “optimum clearance” range from 100µm to 400µm+.2,5,6 Recent studies have shown that in corneas without endothelial dysfunction, the value doesn’t seem to matter, as long as corneal clearance is present to some degree.5,6 Most studies agree that the average corneal swelling is just under 2% after eight hours of scleral lens wear, even in patients with a mean central vault of ~350µm, which is less than the 4% of natural corneal swelling that occurs while sleeping. Another study showed that vault has no impact on visual acuity or scleral lens success in patients with dry eye.5,6
On the flip side, a recent study found that endothelial blebs, or the “transient disappearing of corneal endothelial cells,” occur after the first 15 to 25 minutes of scleral wear.7 This phenomenon was evident with a corneal vault of 400µm but not 200µm. This implies that there may be increased strain on the endothelial surface with increased corneal vault in scleral lens wear. Same-day exams—where a lens is placed on the eye and the patient wears it for several hours before assessment of the corneal response to the physiologic stress induced by the lens—can be very helpful.
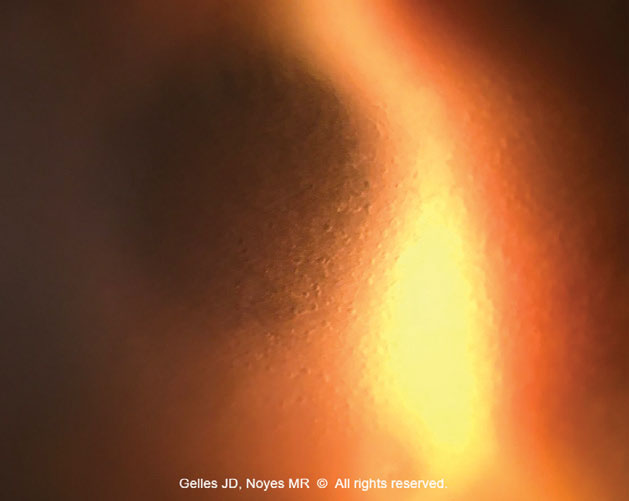 |
| Fig. 3. Scleral lens-induced corneal edema in a case of compromised endothelial health. Click image to enlarge. |
Takeaways
The scleral lens reservoir is key in providing optimal optics and nourishing the ocular surface. These tips can help effectively troubleshoot common issues and sequelae related to the lens reservoir for a more successful fit. Baseline testing, documentation and evaluation after lens removal are paramount in maintaining or improving corneal health. It can be easy to chase the “perfect scleral lens fit,” but don’t lose sight of the eye underneath.
1. Schear MJ, Ibrahim K, Winokur J, et al. Treatment limitations with PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem): one center’s experience. Eye Contact Lens. 2019;45(5):315-7. 2. Barnett M, Courey C, Fadel D, et al. CLEAR—Scleral lenses. Cont Lens Anterior Eye. 2021;44(2):270-88. 3. Fadel D. Scleral lens issues and complications related to a non-optimal fitting relationship between the lens and ocular surface. Eye Contact Lens. 2019;45(3):152-63. 4. Kumar M, Shetty R, Khamar P, Vincent SJ. Scleral lens-induced corneal edema after penetrating keratoplasty. Optom Vis Sci. 2020;97(9):697-702. 5. Rathi VM, Mandathara PS, Dumpati S, Sangwan VS. Change in vault during scleral lens trials assessed with anterior segment optical coherence tomography. Cont Lens Anterior Eye. 2017;40(3):157-61. 6. Sonsino J, Mathe DS. Central vault in dry eye patients successfully wearing scleral lens. Optom Vis Sci. 2013;90(9):e248-51. 7. Giasson CJ, Rancourt J, Robillard J, et al. Corneal endothelial blebs induced in scleral lens wearers. Optom Vis Sci. 2019;96(11):810-7. |


