  |
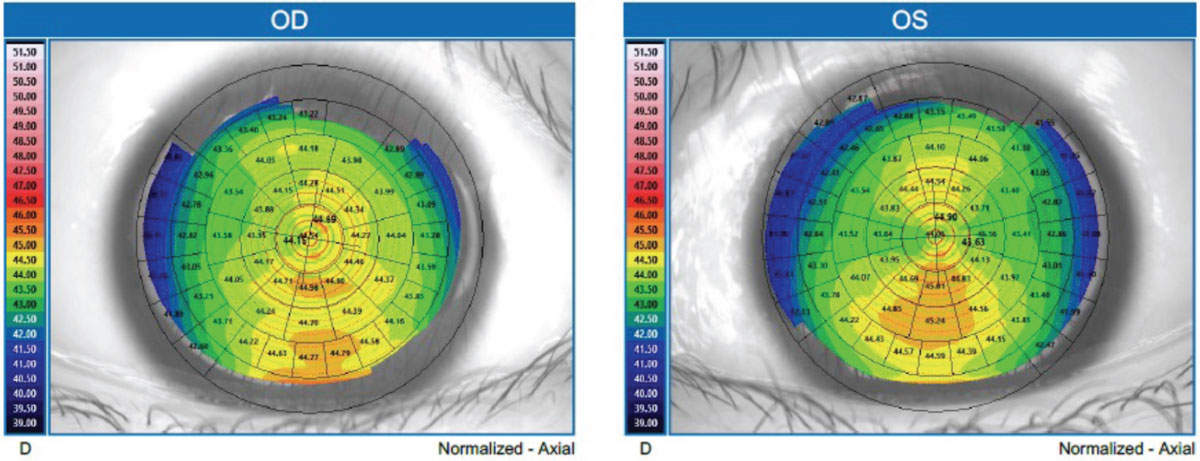
A 10-year-old Chinese girl presented for a prescription check. She reported recent concerns about gradual blurriness in her distance vision. Her entering visual acuity (VA) was 20/40-2 OD and 20/40 OS. Her last comprehensive eye exam, conducted four months prior, revealed a prescription of -1.75sph OD and -1.25-1.00x180 OS. Following cycloplegic refraction, her updated prescription was determined as -2.50sph and -2.00-0.75x180 with a best-corrected VA of 20/20 OU. Placido disc topography (Myah, Topcon) showed an average keratometry reading of 44.42D and 44.23D in the right and left eyes, respectively (Figure 1). Furthermore, axial length measurements were compared, noting an increase from 24.35mm to 24.58mm OD and from 24.21mm to 24.39mm OS over the same four-month period.
 |
|
Fig. 1. Topography of the patient’s right and left eyes. Click image to enlarge. |
Considerations
Here we highlight our thought process and consider how we would proceed:
Dr. Su: Given the moderate prescription change and a 0.2mm axial length shift observed within a short span, it’s imperative to initiate a dialogue with both the patient and parents or guardian about the implementation of myopia control. At 10 years old and with several years of ocular development ahead, it’s crucial to emphasize the significance of slowing down progressive myopia by subsequently slowing down axial length elongation. Our primary aim is to prevent progressive myopia and mitigate the risk of irreversible eye disease in the future.
There are a range of myopia control methods, including orthokeratology (ortho-K), multifocal soft contact lenses (CLs), low-dose atropine drops and combination therapies. Fortunately, as a practitioner in Canada, I have access to myopia control spectacles as well. To determine the most suitable approach, I would assess the patient’s and parents’ lifestyle factors. Is the child involved in sports such as swimming or gymnastics? Do the parents prefer to be actively involved in lens care?
The patient presents with -1D of cylindrical correction in the left eye. While current FDA-approved dual-focus multifocal soft CLs can accommodate low levels of astigmatism, I would lean towards initiating treatment with ortho-K. Additionally, I would advocate for getting a backup pair of myopia control glasses in the cases of lens issues or the need to discontinue lens wear temporarily. I would also engage in discussions with the patient and parents about lifestyle adjustments, such as increasing outdoor activities and taking regular breaks during prolonged near work. Close monitoring and regular assessment of axial length are paramount in this process to check for efficacy of the treatment.
Dr. Pfeifer: When this much change in prescription and axial length is seen in less than one year, alarm bells should be going off in the practitioner’s head. The amplitude of these alarms should only get louder with younger patients—such as in this case. This patient’s eyes are growing too fast and she has many years of development left, so one can only guess how long the eyes may become. The conversation of slowing down the progressive axial length elongation to protect this patient’s vision needs to be had with this patient and her family.
Luckily, we currently have many options for slowing axial length elongation. Various factors, both ocular and non-ocular, influence the likelihood of success of these options. Patients involved in activities such as sports or dance may wish to pursue a spectacle-free option, whereas kids who may not have ideal hygiene may be better off with parents instilling atropine every night. Of the ocular factors, corneal curvature plays the largest role, especially in CL options. Success in ortho-K relies on average-to-steep corneal curvature with a low-to-moderate amount of astigmatism. Elevated corneal astigmatism can also reduce the availability of center distance multifocal CLs. This is less of a factor with glasses designed to slow axial length elongation, although they are not yet available in the US, which is something that parents should be aware of as an potential future option. Atropine is typically viewed as a catch-all treatment option, as the main contraindication is an allergy and children typically don’t suffer from increased glare.
This patient would be a great candidate for ortho-K, so that would be my ideal choice of treatment. With her corneas possessing curvatures on the steeper side of average and her corneal astigmatism relatively matching her refractive astigmatism, she would likely attain great vision with a well-centered treatment zone. If the patient does not wish to pursue ortho-K at this time, soft center-distance multifocal CLs would be my secondary choice. I would stress the importance of taking breaks from near work and to get outside every day as well. I would also reassure the parents that the patient will be regularly followed every six months to monitor for progression and to alter or add treatment modality if any unwanted change occurs.
Dr. Noyes: My practice only provides care for patients needing medical CLs for severe corneas and ocular surface disease. We do not provide ortho-K or myopia control. I will defer to my colleagues on this one.
Dr. Gelles: This patient is undergoing progressive axial length elongation (PALE), and with the observed rapid changes, it could even be described as precipitous axial length elongation. No matter how it’s described, intervention is necessary. There are four main interventions to slow PALE, all of which are well-supported by the literature: atropine, defocus soft lenses, ortho-K and various myopia-specific spectacle lenses. In this case, how do I choose what is best for the patient? My biggest question when selecting PALE treatment is always, “What does the cornea look like?” Myopia is a sum of its parts, the most impactful being axial length and corneal curvature. The pediatric population is where PALE and keratoconus overlap, so it is important to evaluate the cornea to know before you treat.
The way I approach myopia control is similar to the way a surgeon approaches refractive surgery. If the cornea is normal and the prescription is within reasonable parameters, I will initiate a corneal-based treatment with ortho-K. If the cornea is suspicious, I will initiate a non-cornea-based treatment with atropine, defocus soft lenses and/or spectacle lenses, which will preserve the anterior corneal metrics for comparison over time. I use corneal tomography to evaluate these patients, as Ks are grossly inadequate for corneal evaluation and topography is not sensitive enough to catch the earliest signs of keratoconus (thickness and posterior corneal metrics) which are critical in this population. A recent US-based study using corneal tomography to screen pediatric patients found a high prevalence of keratoconus and keratoconus suspects—a combined prevalence 1:223.1
In this patient, the topography images may not be the most reliable on the right eye since motion blur can be seen in the image, but the left appears to be better quality without evaluating the mires image. In both topography maps, there is slight asymmetry from inferior to superior; on the OS at the 6mm OZ it appears to be about a 1.5D asymmetry. This is suspicious and warrants further investigation with corneal tomography to specifically evaluate anterior and posterior elevation, thinnest point and global pachymetry change across the cornea, as well as epithelial thickness metrics to determine if keratoconus is present. If decisions are going to be made based on this topography data alone, in an abundance of caution, I would start with defocus soft lenses and monitor the patient at three- to four-month intervals with emphasis on evaluating the cornea for changes. If PALE was still progressing at a higher than normal rate, I would add 0.05% atropine.
The use of other CL options, such as hybrid, corneal gas permeable or scleral lenses, with simultaneous multifocal optics could be used to deliver the myopic defocus optical profile with the potential advantage of masking corneal astigmatism; however, unlike the other options, this has not been thoroughly studied and well-established and would be my last resort.
Discussion
Progressive myopia can be managed in several ways and selecting the right treatment requires a personalized approach. The primary goal is to reduce the risk of visual impairment. While slower prescription changes are also desirable, they are just an added benefit. Age, genetics, environment, maturity, daily activities and parental involvement all influence the choice of intervention. Frequently, questions about the safety of CL wear in the pediatric population arise. The risk benefit comparing the risk of microbial keratitis to the lifetime risk of severe visual impairment as a result of high myopia (>6.0D) or long axial length (>26mm) in children undergoing myopia control treatment with CLs and ortho-K is in favor of treatment with both options.2
Following these patients at short intervals—typically every three to six months—is important, as changes can happen rapidly and axial length gained cannot currently be undone. Monitoring these patients takes more than a phoropter and keratometer. Devices such as a topographer and biometer are essential for effective monitoring. Myopia is a sum of its parts, so ensuring corneal stability and directly measuring axial length is critical.
Results
During the initial visit four months prior, a discussion about myopia control was had with the patient and her parents. At that time, they opted to postpone any further action until the following year, feeling that the patient was comfortable with her current spectacles. Upon revisiting the topic at a later point, both the doctor and parents agreed that ortho-K would be the most suitable option, especially considering the patient’s regular swimming routine of four days a week.
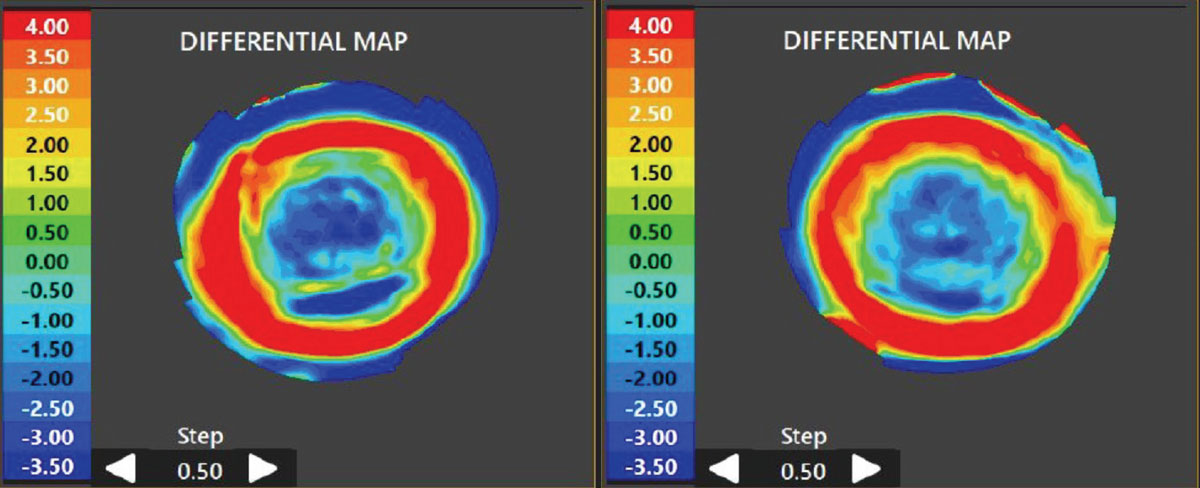
Ortho-K lenses (Moonlens Flex, Precision Technology Services) were ordered and the patient underwent follow-up appointments at one day, two weeks and one month post-wear. By the one-month follow-up, the patient reported excellent vision throughout the day without any complaints. The topography comparison map revealed a well-centered treatment zone (Figure 2). The lenses were removed and there was no staining to the cornea. Additionally, due to the family’s frequent international travels and concerns about potential loss of CLs, they opted to add myopia control glasses as well, equipped with Highly Aspherical Lenslet Technology (Stellest, Essilor). Axial length measurements were scheduled every three months to monitor progress. At the six-month follow-up, both the patient’s prescription and axial length remained stable.
 |
|
Fig. 2. Comparison map of pre- and post-wear topography scan, highlighting the change in corneal shape caused by ortho-K. Click image to enlarge. |
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.
1. Harthan JS, Gelles JD, Block SS, et al. Prevalence of keratoconus based on Scheimpflug corneal tomography metrics in a pediatric population from a Chicago-based school age vision clinic. Eye Contact Lens. 2024;50(3):121-5. 2. Gifford KL. Childhood and lifetime risk comparison of myopia control with contact lenses. Cont Lens Anterior Eye. 2020;43(1):26-32. |


