  |
A 20-year-old Caucasian male presented to the clinic as a referral from our cornea service for trauma-induced corneal scarring of the left eye. He was launching fireworks with his friends when one “didn’t go off.” He picked it up to inspect the problem and the firework exploded in his hand, resulting in chemical, thermal and shrapnel-based trauma to the left eye.
Considerations
Here, we highlight how we would proceed.
 |
|
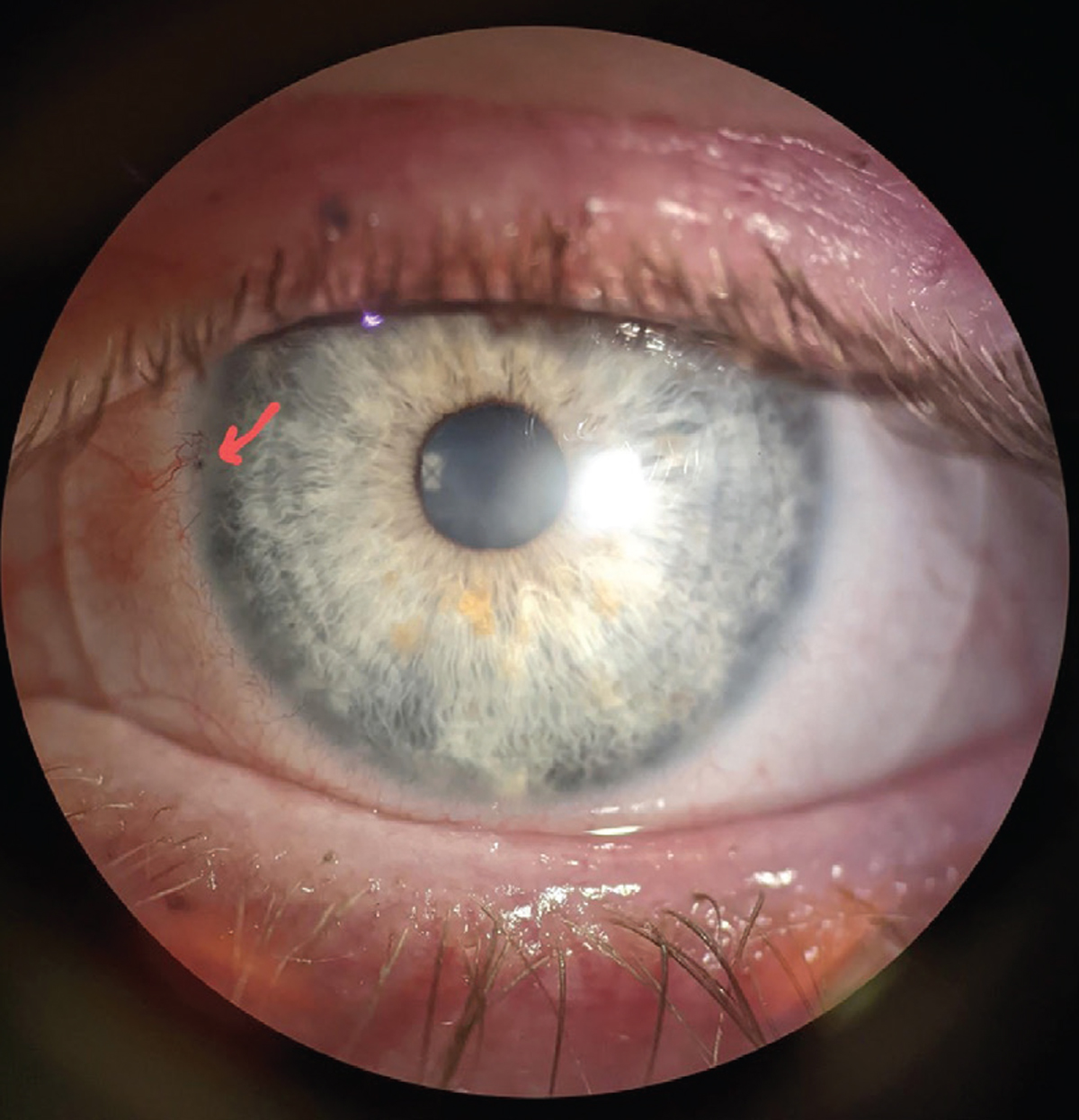
Soot is evident in the limbus (red arrow). Click image to enlarge. |
Dr. Noyes. I think the first thing to consider in a case like this is evaluation of the ocular surface with sodium fluorescein (NaFl). One key aspect that drives the decision behind which contact lens modality to pursue is the health and integrity of the corneal limbus, especially in trauma or chemical burns. If a patient exhibits any signs of limbal stem cell deficiency (LSCD), this could limit your treatment options, as rubbing on the affected area will worsen findings such as scarring, neovascularization and pannus, and likely promote further stem cell morbidity.
If the corneoscleral limbus looks acceptable, then any choice of contact lens could potentially be an option. If LSCD is present, scleral options are usually the best choice, as they are the only option that completely vaults the limbus while also providing hydration, staving off potential future problems. In some cases, you may be able to get by with a corneal gas permeable lens; however, heed caution that the lens has a small enough diameter where either (1) it does not cross the limbus or (2) the point at which it crosses the limbus is further away from the affected area.
Dr. Gelles. After evaluating the integrity of the limbus, determining the severity of the irregularity can provide lots of options for this patient. If the irregularity is minor, great options will include soft, custom soft, corneal gas permeable and hybrid lenses. For those with more severe irregularity, scleral lenses and piggyback systems are my go-to. Trauma cases like this can be challenging, and addressing the patient’s chief complaint may not be as simple as masking the irregular surface.
Depending on the severity of scarring that is present, it’s possible the glare the patient is describing is not actually aberration from an irregular corneal shape but rather scatter from stromal scarring.
Aberrations can be addressed with a rigid lens, and residual aberrations can be further addressed with wavefront-guided optics, currently only available for scleral lenses. But with scatter, the only way to really improve vision further is to clear the media with surgical interventions, which in this case would be a superficial keratectomy, phototherapeutic keratectomy and anterior lamellar keratoplasty. Several case studies have reported on scleral lenses reducing corneal opacity over time, making this an excellent option for this individual. Try going the non-surgical route first; if no visual improvement is noted, move on to weighing surgical considerations.
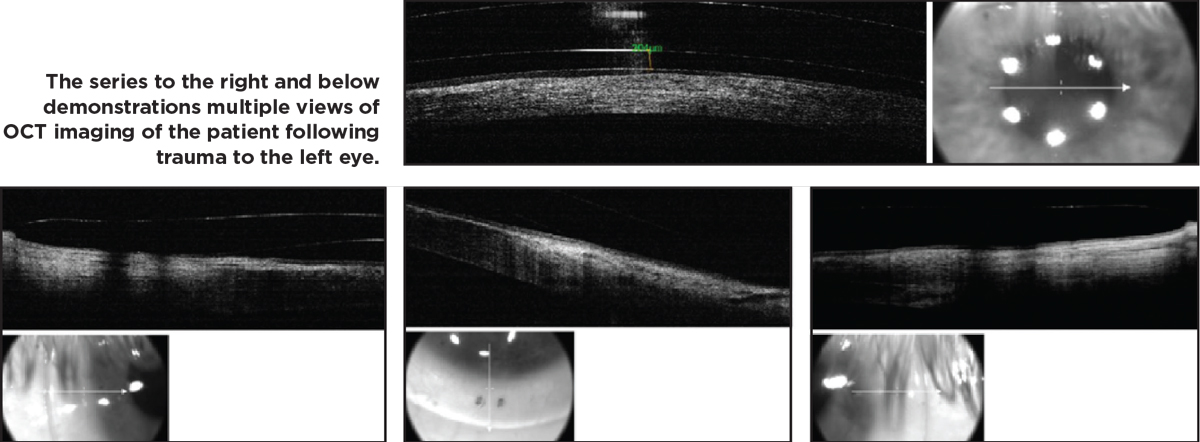 |
| Click image to enlarge. |
Discussion
There are several ways to evaluate aberration vs. scatter, including a rigid lens over-refraction, wavefront aberrometry and even glare testing, the latter of which is the same as you would perform during a cataract evaluation. If glare is resolved by a rigid lens over-refraction, then it’s all aberration. If not, use a wavefront aberrometer to measure the residual aberration, and remember to evaluate the spot diagram. The spacing or displacement of the spots relative to a normal grid indicates aberration vs. scatter, which is the quality of the individual spot and should correspond with the location of media opacities. There are forms of visual quality evaluation that can deliver an objective scatter index number quantifying the spot quality.
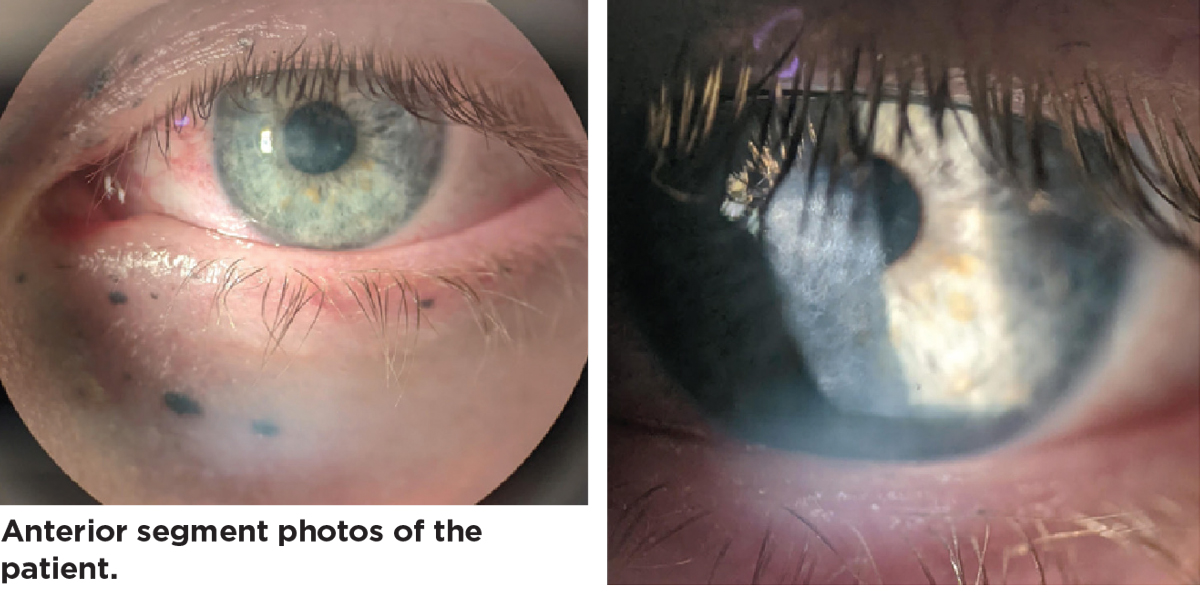 |
| Click image to enlarge. |
Finally, glare testing with a brightness acuity test is also an option. If vision is reduced with this method, then it can be concluded that there is a significant amount of scatter affecting the patient’s vision.
Results
This patient exhibited signs of LSCD in the left eye, and his slit lamp exam and tomography imaging determined his scleral shape and corneal surface to be moderately irregular. These factors led to the decision to fit him with a scleral lens in the left eye only.
A freeform, ocular impression-based scleral lens (EyeFitPro, Eye Print Prosthetics) made from ultra-high Dk material (Optimum Infinite, Contamac) was designed for the patient. The 17.5mm diameter combined with the freeform shape allowed for excellent alignment to the irregular scleral contour without compression and with full limbal clearance, as well as rotational and translational stability. With this lens, the patient was able to achieve 20/20 vision with complete resolution of his glare issues and improvement in LSCD signs.
Want to Have Your Case Evaluated in the Next Issue? Submit your case, complete with history, imaging and results, to [email protected] with the subject line, “Noyes and Gelles Troubleshooting.” In an upcoming issue, Drs. Noyes and Gelles will weigh in on how they would each handle the case.


