 |
A 79-year-old male presented for a contact lens fit after a regraft penetrating keratoplasty (PKP) of the right eye, with two sutures remaining. He presented without complaint of discomfort or change in vision but noted increased foreign body sensation for the past week. The two sutures had both eroded and both had surrounding infiltrates. The sutures were removed and he was started on moxifloxacin QID. At a one-week follow up, the infiltrates had resolved and there was no epithelial defect. He was fit into a gas permeable lens.
Corneal sutures pose a risk for infiltrative keratitis, with one study showing 3.6x increase in a graft infection when sutures are present.1 These sutures are typically made from nylon, which is classified as non-absorbable, but these sutures do biodegrade over time and will progressively lose tensile strength. They loosen and may rupture. Corneal sutures are typically removed (or break) within two years.1 Longer suture presence increases the risk of a keratitis event, with one report showing a 71.6% incidence over four years.3 Ocular surface disease (strongly), regrafts, glaucoma and herpes simplex keratitis (weakly) all increase the odds of developing suture-related microbial keratitis.4
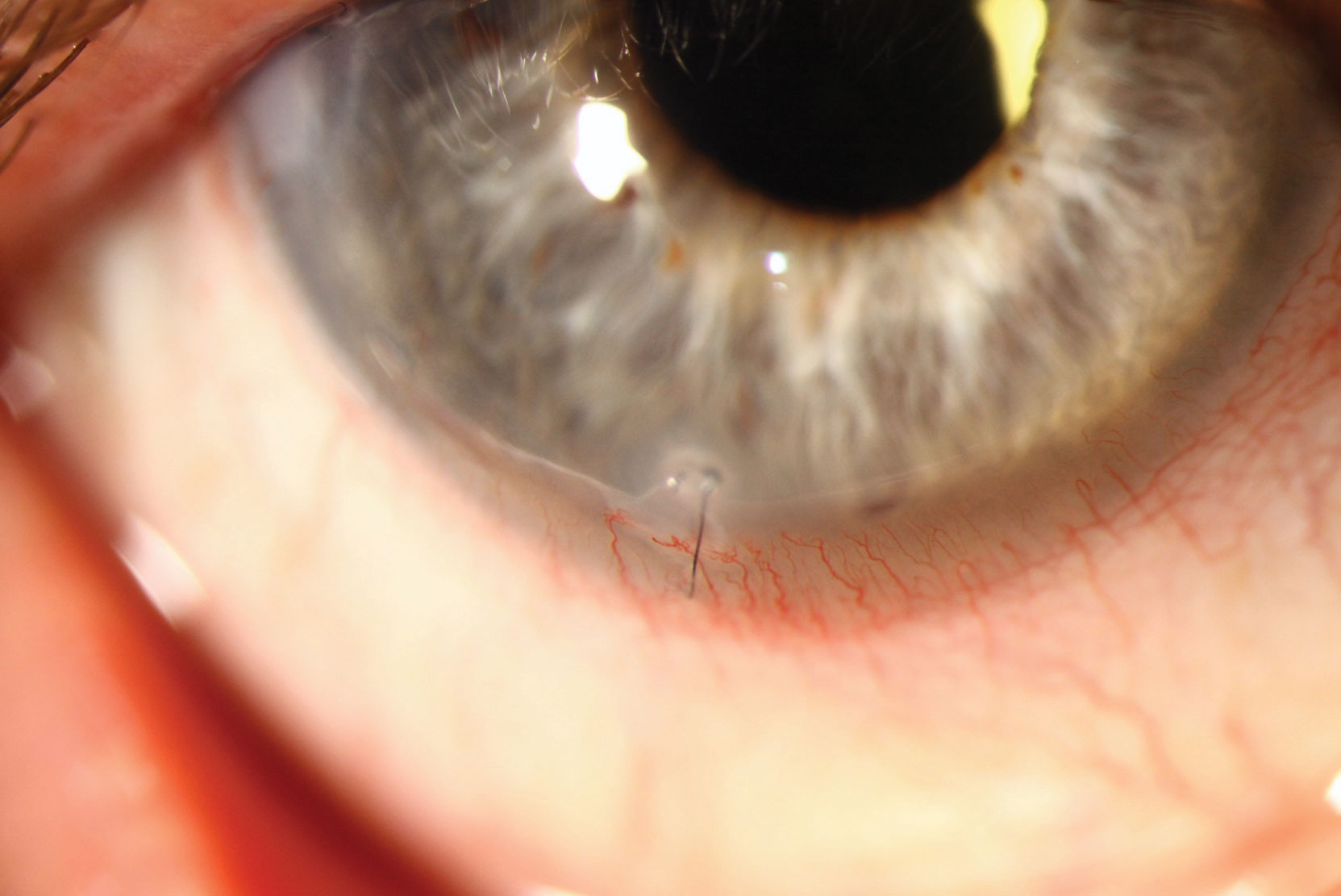 |
| Monitor corneal sutures closely, as they provide a vector for infection. Click image to enlarge. |
Gram-positive cocci (e.g., Staphylococcus aureus and epidermidis) are the most commonly isolated organisms of exposed sutures, while gram-negative organisms (e.g., Moraxella) are more common in the absence of sutures. Polymicrobial infections are common.
Nylon suture materials can harbor biofilms—a complex mixture of different bacterial organisms encased in a protective coating. Bacteria in biofilms are significantly more resistant to antibiotics.
Corneal sutures act as a nidus for the colonization of pathogens, which promotes the invasion of a compromised epithelial surface. If an unusual pathogen is not suspected and there is no evidence of endopthalmitis, a broad-spectrum antibiotic, with good gram-positive cocci coverage, is recommended. Suture removal is important in order to eliminate the scaffolding of microbial invasion and biofilm formation. Patients should be followed closely to monitor resolution of the disease.
| 1. Vajpayee RB, Boral SK, Dada T, Murthy GVS, Pandey RM, Satpathy G. Risk factors for graft infection in India: a case-control study. Br J Ophthalmol 2002;86: 261-65. 2. Jackson H, Bosanquet R. Should nylon corneal sutures be routinely removed? Br J Ophthalmol 1991;75:663-64. 3. Wagoner MD, Al-Swailem SA, Sutphin JE, Zimmerman MB. Bacterial keratitis after penetrating keratoplasty: incidence, microbiological profile, graft survival and visual outcome. Ophthalmology 2007; 114:1073-79. 4. Moorthya S, Grauea E, Jhanjiab V, Constantinoua M, Vajpayee RB. Microbial keratitis after penetrating keratoplasty: impact of sutures. Am J Ophthalmol 2011;152:189-94. |


