 |
A 72-year-old white female, presenting for a cataract evaluation, was subsequently referred for a scleral lens evaluation due to fluctuating vision. She was told by her previous doctor that nothing could be done about her vision, so she has lived for many decades with poor vision and without seeking care. She recently had been experiencing greater swings in her vision and thought perhaps cataract surgery would help.
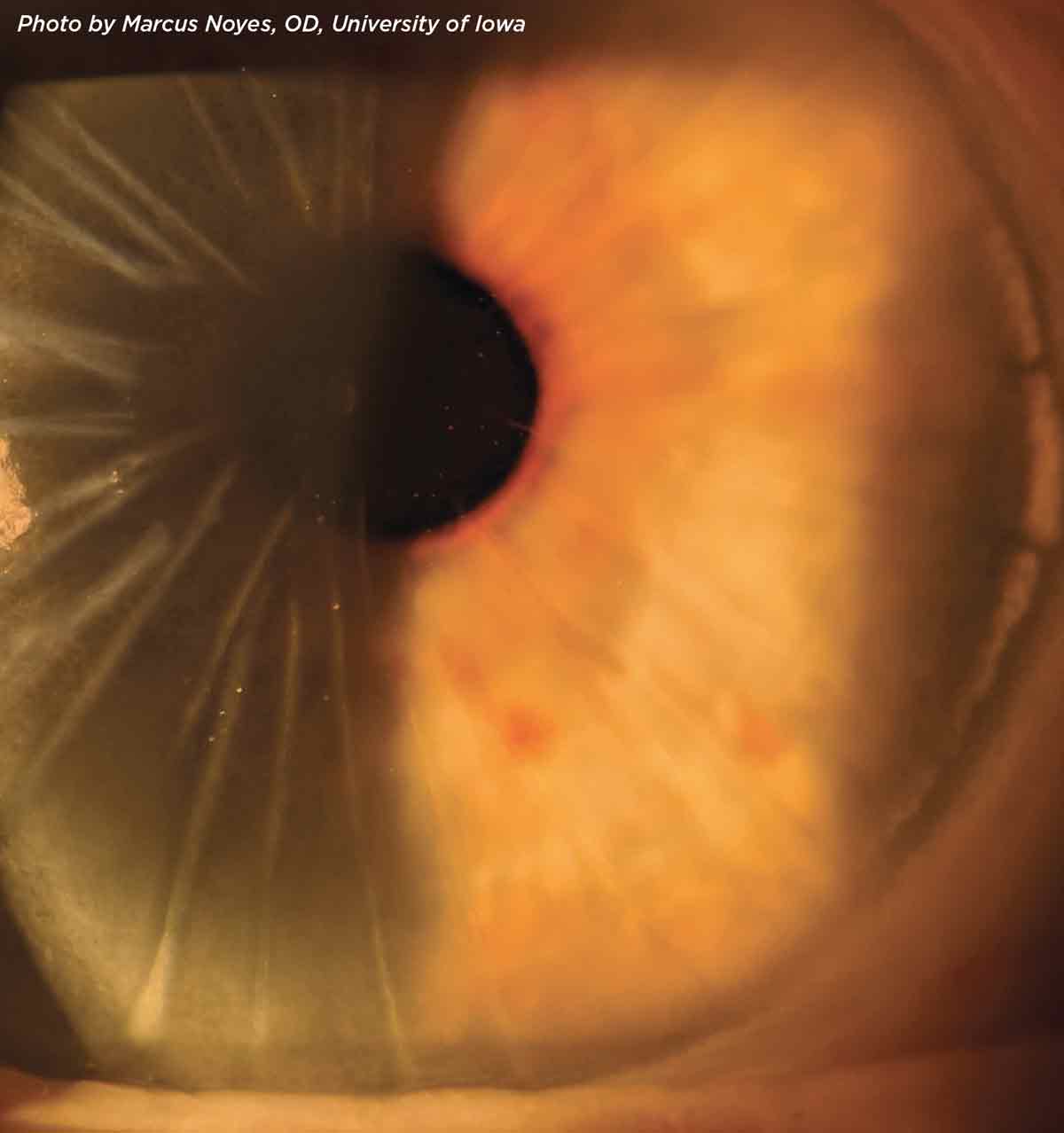
She presented with visual acuities of OD 20/60 and OS 20/40. Slit lamp examination revealed 42 linear radial incisions in each eye, with ferrous staining in the central optic zone. She had mild, non-surgical cataracts. A trial of scleral lenses yielded 20/25 vision in each eye. No historical refractive data was available.
Radial keratometry, a popular refractive procedure throughout the 1980s and early 1990s, was effective in flattening the cornea through a series of radial incisions into the stromal bed. The number of cuts (typically eight) and their depth (typically 80% to 90%) affected the resultant power. By the early 2000s, it was supplanted by the more predictable laser refractive procedures.
 |
|
Click image to enlarge. |
We have dealt with numerous complications in the decades following the RK boom, including dry eye, biomechanical instability at the incision points (leading to unstable irregular astigmatism), progressive localized corneal flattening or steepening with resultant hyperopic or myopic refractive shifts, increased higher-order aberrations, incisional infections, epithelial down-growth and even globe rupture.
Many RK patients are now at an age where cataracts are a concern. Outcome predictability is highly variable. Cataract surgery increases the risk of incision dehiscence and refractive instability. There are also case reports of collagen crosslinking exacerbating the wound instability, with the hypothesis that crosslinking does not reach deep into the incision, resulting in changes to, rather than stabilizing of, the existing scars.
As in this case, refraction is difficult and often shifts the aberrations without increasing overall visual acuity. This is frustrating for both patient and doctor. Patients are often referred for contact lens fitting prior to surgery, since surgical outcomes are so highly variable. Most often, scleral lenses are used for post-RK corneas because the extreme flatness and irregular astigmatism may be difficult to fit with a corneal lens. While the cornea may continue to fluctuate under a scleral, the lacrimal lens will neutralize surface irregularity and provide stable vision. GP lenses tend to decenter; piggybacking is recommended for better centration and to avoid bearing on elevations.
This patient chose to continue without visual correction and to use reading glasses as necessary. She had habituated to her visual world and preferred not to hassle with contact lenses, since her original goal was to be correction-free.


