 |
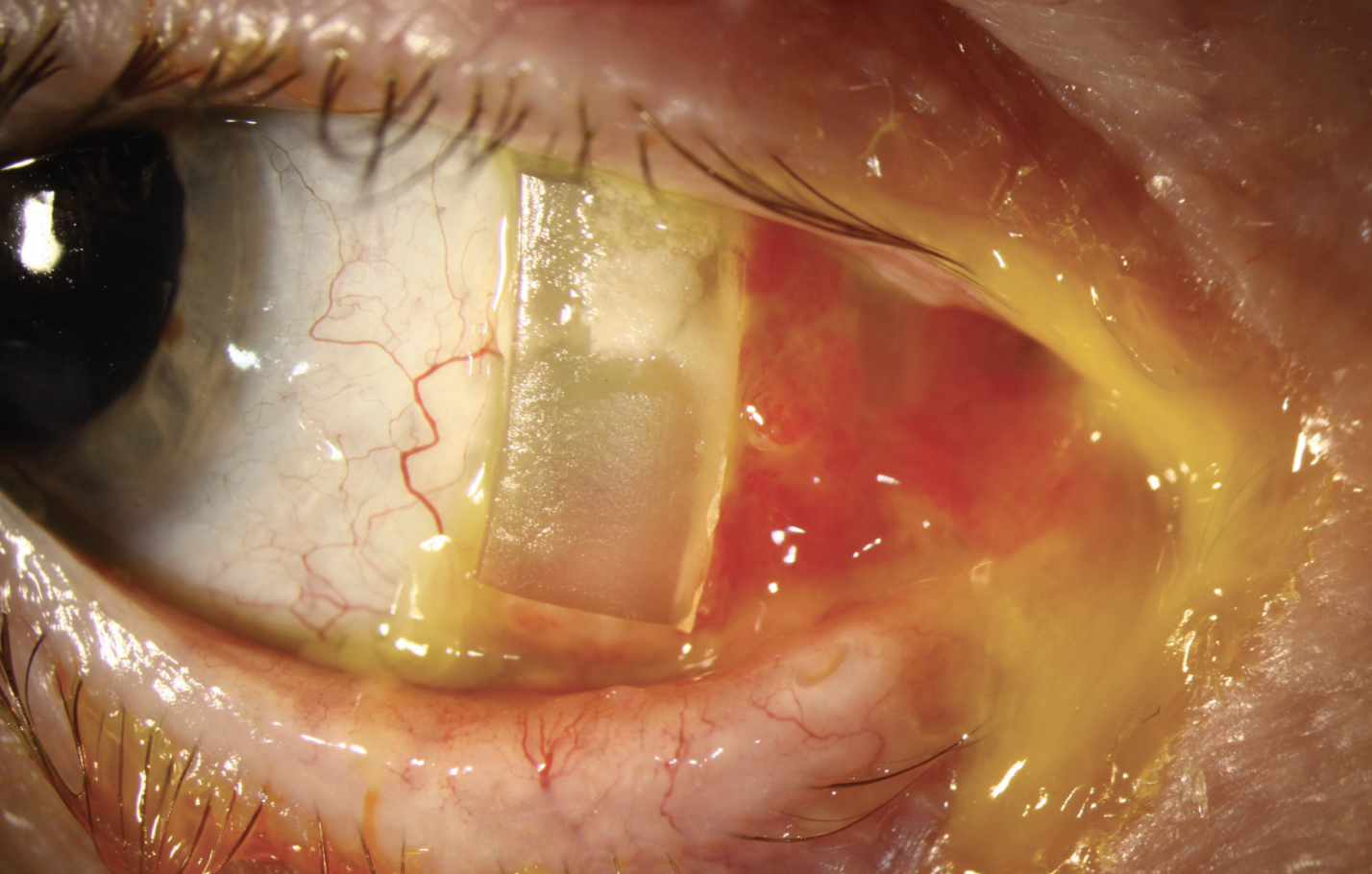
A 66-year-old male presented with a complicated ocular history starting with a scleral buckle procedure in the right eye 40 years prior. He later underwent LASIK (in its early years) for the anisometropia and developed ectasia with 20/150 BCVA. Due to progressive visual field loss, he was diagnosed with glaucoma. However, because of breathing issues, a Baerveldt implant with scleral patch graft was placed in hopes of getting him off beta-blockers.
Subsequently, while hospitalized for respiratory failure, he was diagnosed with Wegener’s granulomatosis and developed peripheral ulcerative keratitis and necrotizing scleritis with superficial erosion at his tube site. He was diagnosed with neurotrophic scleral keratitis OD and a lateral tarsorrhaphy was placed, which maintained conjunctival coverage for nearly a decade.
 |
|
Click image to enlarge. |
However, he eventually complained of increasing discomfort—the buckle was extruding nasally. It was removed without disruption to the tube shunt. The patient was referred for placement of a scleral cover shell for protection of the ocular surface and vision correction. An impression-based lens device was designed to vault the tube shunt and align with the irregular conjunctiva and he achieved 20/40 vision.
Wegener’s granulomatosis, now called granulomatosis with polyangiitis (GPA), is an uncommon autoimmune disorder characterized by asthma, blood and tissue eosinophilia, and small-vessel vasculitis. It is often associated with kidney and lung involvement but can affect any small vessels. Up to 60% of patients have ocular involvement, which can include episcleritis, scleritis, conjunctivitis, keratitis, uveitis, retinal vasculitis, retinal arterial or venous thrombosis, retinal exudates, retinal hemorrhages, blurred vision, blindness, proptosis and orbital granulomatous masses and epiphora.
GPA is considered an autoimmune disease with a prevalence of 1:20,000, with a predilection for Caucasians with Northern European descent. It affects both sexes equally. Treatment includes a combination of glucocorticoids, cyclophosphamide and rituximab, achieving remission in 80% to 90% of patients. Our patient is maintained on oral prednisone and rituximab.


