|
An 84-year-old Caucasian woman presented for evaluation of “fuzzy vision.” She had a history of bilateral sequential anterior ischemic optic neuropathy with no subsequent recovery of vision. She denied symptoms of giant cell arteritis. Medical history was significant for hypertension, hyperlipidemia and Atrial fibrillation. Her current medications included metoprolol, coumadin, amlodipine and amiodarone.
 |
|
Click image to enlarge. |
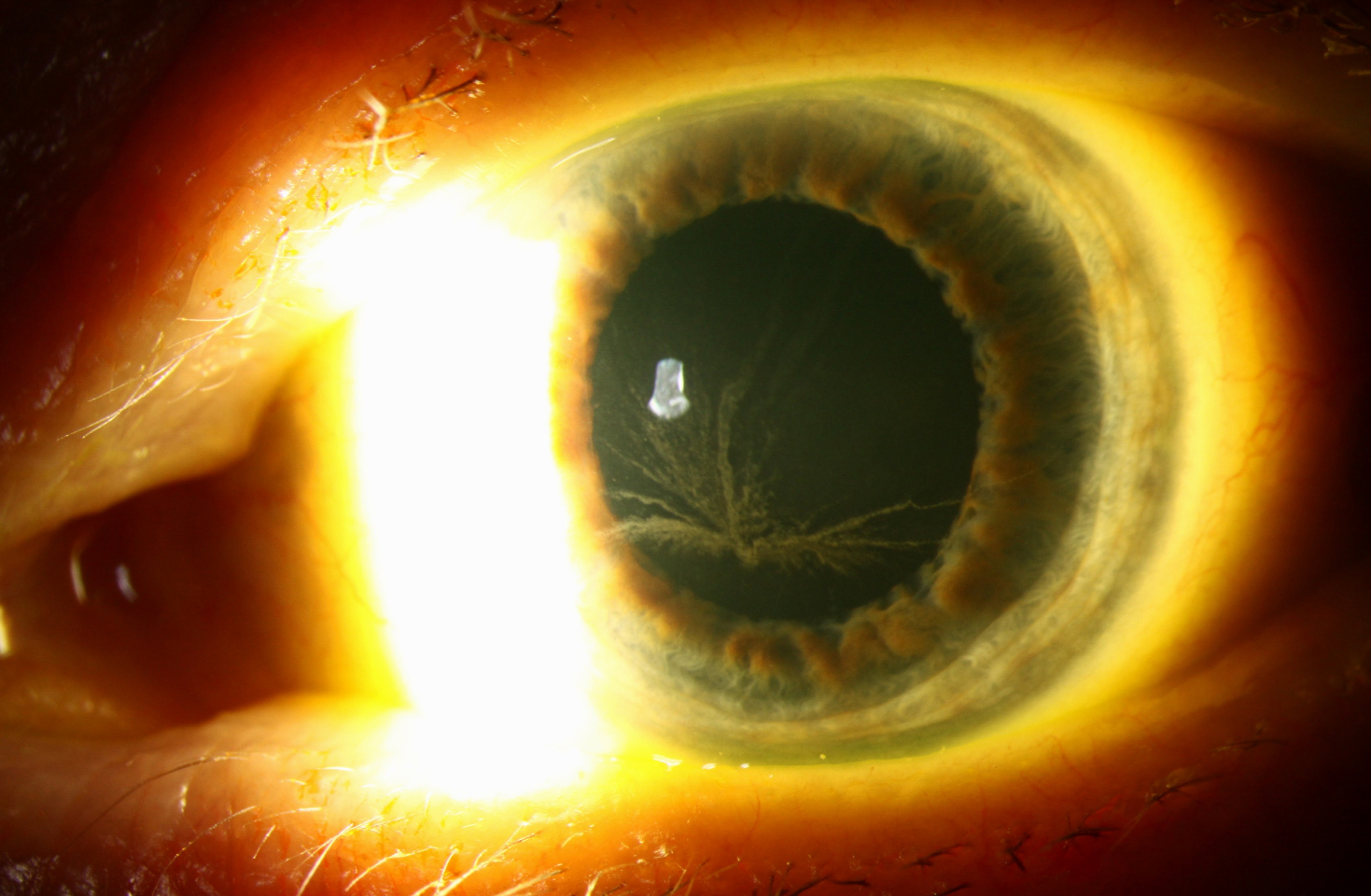
Exam revealed visual acuities of 20/30 OD and HM OS, with a 1.2-1.5 log unit RAPD OS. Anterior segment exam revealed vortex keratopathy OU and 2-3+ nuclear sclerotic cataracts with cortical cataract OU.
Dilated exam revealed a hazy view to the fundus OU. There was bilateral optic disc pallor with cupping, OS>OD, with soft drusen in the maculae OU. Critical flicker fusion was moderately decreased OD and could not be obtained (due to poor vision) OS. Visual fields revealed an inferior altitudinal cecocentral scotoma with inferonasal constriction OD and a dense cecocentral scotoma with nasal constriction OS. Compared to past exam, visual field differences were mainly due to changes on the total deviation rather than pattern deviation, likely due to refractive change or media opacity rather than significant progression of her optic neuropathies.
Amiodarone treats cardiac dysrhythmias; all patients taking this drug will develop corneal verticillata (vortex keratopathy). Patients are generally asymptomatic, although some complain of halos. Verticillata appear as fine grey-brown opacities in a whorl-like pattern, branching out from the inferior cornea. The drug deposits happen at the level of the basal epithelium. While the deposits will fade if the drug is stopped, generally it is not recommended to alter systemic treatment in response.
Our patient was advised that her inflammatory markers are within normal limits and, based on our ocular findings, we did not advise a change in her meds.