 |
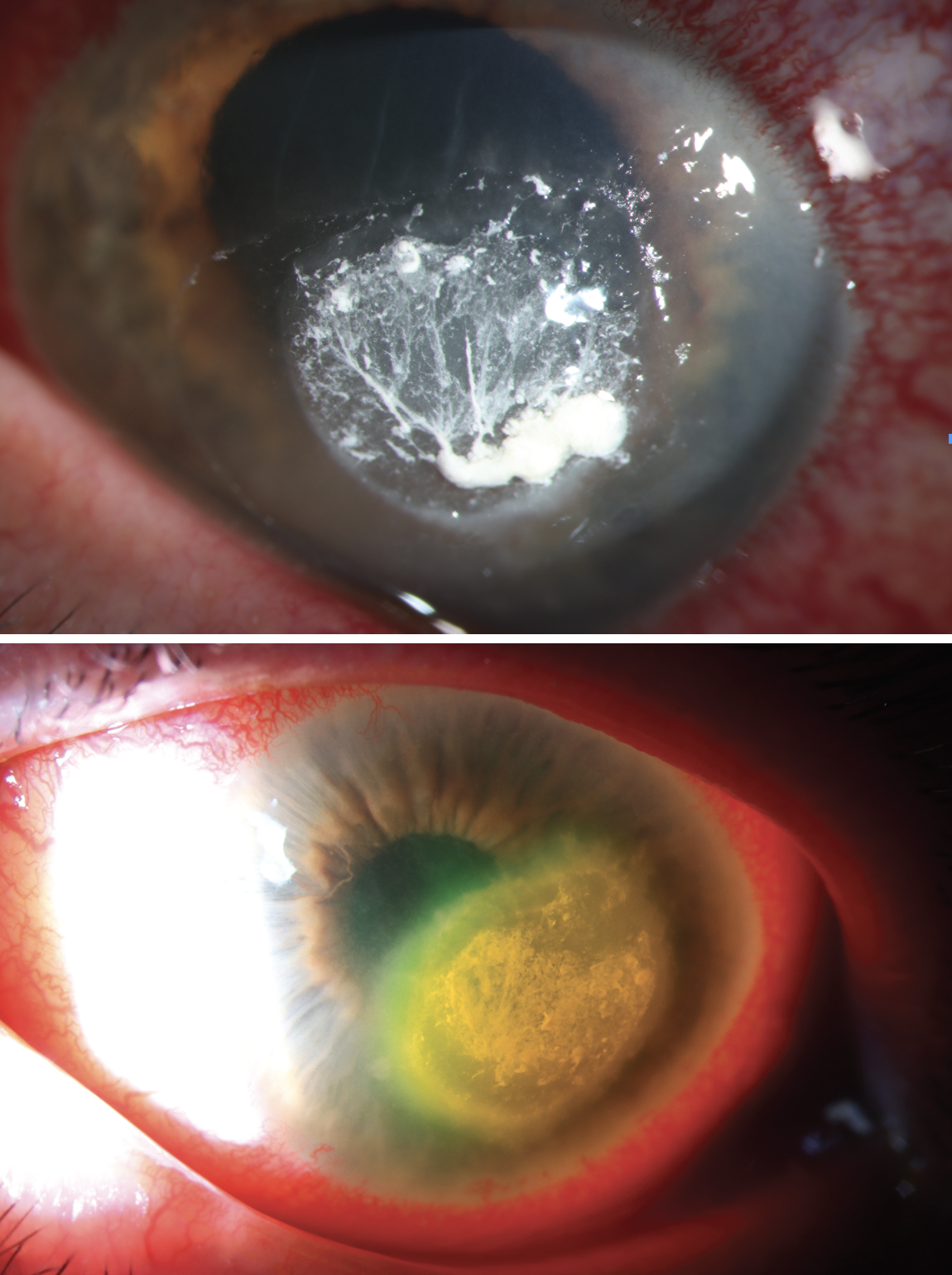
A 57-year-old contact lens wearing male presented with a corneal ulcer OS. He was doing yard work and said he may have gotten something in his eye. The next day, he noticed irritation and difficulty focusing. His local optometrist started him on moxifloxacin and cyclopentolate OS. As irritation and blurred vision continued to worsen, a local ophthalmologist added erythromycin and valacyclovir. Three days later he lost vision in the left eye and was referred to a cornea specialist, who added fortified vancomycin and fortified tobramycin. When he did not improve, he was referred to the ED.
In our hospital-based ophthalmology department, corneal scrapings stained positive for fungal elements. He started on topical natamycin and oral fluconazole. Two days after, he felt improvement with less pain. Although the epithelial defect was smaller, he had mild corneal melting, so medroxyprogesterone was added.
 |
|
Click image to enlarge. |
Fungal keratitis is a challenge to diagnose and treat. Over 100 fungal species have been implicated, the most common being Fusarium, Candida and Aspergillus. Candida predominantly invades pre-existing epithelial defects, while filamentous fungi are commonly implicated in post-traumatic infections. Risk factors for fungal ulcer include contact lens wear, ocular surface disease, topical steroid use, atopic disease and trauma (specifically exposure to vegetative matter).
Fungal origin should be suspected any time there is an unusual presentation of keratitis not responding to therapy. It may appear as stellate lesions with an intense inflammatory response and tissue necrosis. Fungi can also infiltrate the sclera and induce scleritis and pan-ophthalmitis, or breach Descemet’s and cause fungal endophthalmitis.
Definitive diagnosis is made with Giemsa or Gram stains, although PCR and confocal microscopy are also sensitive techniques. It is also prudent to PCR test for HSV and confocal/scrape for Acanthamoeba at presentation.
Natamycin 5% is first-line treatment. Voriconazole 1%, considered to have better penetration, may be a superior alternative. Steroids are contraindicated due to risk of fungal proliferation. However, medroxyprogesterone was added as a protective agent due to its anti-collagenase activity. It reduces inflammation with less wound repair suppression. There is a high risk for vision loss with fungal keratitis and diagnosis should be made quickly.


