 |
A 24-year-old Asian female presented to our clinic with an ocular history of pain to the left eye that started one month prior. The patient has a history of orthokeratology (ortho-K) wear; no history of eye surgery and no other ocular history was conveyed, as well as no pertinent medical history. Her uncorrected acuity was 20/40 in the right eye.
Prior to our visit, the initial diagnosis was contact lens overuse, which then shifted to possible herpes simplex virus (HSV). The patient was put on ofloxacin QID, erythromycin, ketorolac QID and valacyclovir 1g three times a day. At this time, the patient called her ortho-K practitioner and was also prescribed a steroid eye drop.
At follow-up, the slit lamp exam showed a central ring infiltrate with discrete stromal opacities, centrally and peripherally, along with significant peripheral neovascularization. The patient was cultured for Acanthamoeba, had an HSV PCR and her contact lens was cultured for fungi, bacteria and Acanthamoeba, which came back positive (Figure 1). She reported using tap water to clean her lenses and was sent to our clinic for an in vivo confocal microscopy (IVCM) where cysts were found.
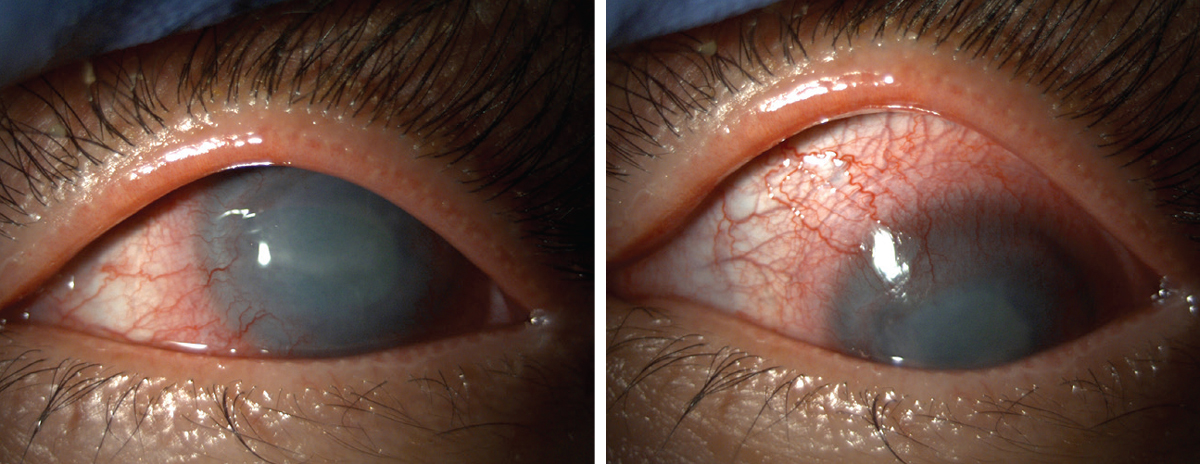 |
| Fig. 1. Acanthamoeba and conjunctival injection shown in our patient. Click image to enlarge. |
The patient was shifted to a regimen of Valtrex (valacyclovir, GlaxoSmithKline) 1000mg BID, ofloxacin and prednisolone (both QID), Impavido (miltefosine, Profounda), PHMB (polyhexamethylene biguanide, 0.02%) and 40mg of oral prednisone a day. As time progressed, an amniotic membrane was used routinely due to dense superficial punctate keratitis and stromal thinning. Brolene (propamidine) QID in the left eye, doxycycline 100mg daily, vitamin C 2g daily and serum tears were also added.
Unfortunately, she continued to worsen and developed an epithelial defect and a white cataract. Now, eight months later, she is still on chlorhexidine 0.02% QID, serum tears QID, vitamin C 100mg, doxycycline 100mg QID and prednisolone TID. She is aware she will ultimately need a penetrating keratoplasty, extracapsular extraction and an intraocular lens OS.
Diagnosis
Acanthamoeba keratitis (AK) is a rare but very serious infection that can lead to vision loss or blindness.1 It is caused by a single-celled living organism—a tiny amoeba called Acanthamoeba—which is found in nature and can be in bodies of water, tap water, whirlpools, air conditioning units and soil.2 In order for AK to grow, the organism has to make direct contact with the eye; a corneal infection will not occur from drinking or inhaling water that has the amoeba in it. Usually, a small scrape or microtrauma on the cornea acts as the vehicle for entry.3
Around 85% of all AK cases in the United States occur in contact lens wearers. Patients who do not store or handle their lenses properly, do not correctly disinfect their cases, swim or shower while wearing lenses are at higher risk.4 Soft contact lens wearers are at an increased risk because Acanthamoeba adheres well to hydrophilic plastic, specifically silicone hydrogels.5
The diagnosis is very challenging and, unfortunately, the available treatment regimens are lengthy—as seen in our case—and not fully effective against all strains. The reason we do not have a better solution is that the pathogenesis of AK is still under study. The combination of common misdiagnosis in most cases and lack of consensus has led AK to remain significant; however, it is still very rare, with an estimated prevalence of 1/100,000 to 9/100,000.6
The first step is to always keep it in your differentials when dealing with a contact lens wearer or any case of trauma involving exposure to soil or contaminated water. Patients may experience extreme pain with photophobia, ring-like stromal infiltrate, epithelial defect and lid edema. AK is usually unilateral and starts off as an epithelial disease that slowly progresses to stromal. If the diagnosis is delayed, the amoeba will have already penetrated further into the corneal stroma, which causes therapy to be difficult. At an early point in AK, one can expect to see diffuse superficial keratopathy, which is why it is often confused with herpes simplex keratitis. Later, multifocal infiltrates will be observed in the stroma, which is confused with fungal keratitis. The characteristic ring infiltrate is only seen in 50% of patients.6
In-office treatments and procedures that can be used to diagnose AK are plate culturing and IVCM. Culturing remains the gold standard for laboratory diagnosis; however, there are several PCR-based techniques that have increased sensitivity.
As previously mentioned, an IVCM was used around one month after this patient’s initial presentation (Figure 2). Acanthamoeba cysts appear on this microscopy as hyper-reflective spherical structures that are well defined by a double wall.5
 |
| Fig. 2. IVCM showed Acanthamoeba cysts at the patient’s follow-up exam. Click image to enlarge. |
Therapeutic Approaches
There are two goals of therapy: (1) removal of the Acanthamoeba cyst and trophozoites and (2) resolution of the host inflammatory response.7
Acanthamoeba trophozoites are sensitive to a variety of available medications: antibiotics, antiseptics, antifungals and antiparasitics. Diamidines and biguanides are the most successful cysticidal antiamoebics. They are usually prescribed in combination and for the first 48 hours, given hourly continuously before being reduce to hourly daytime, then four times a day for up to six months.7
Extracorneal manifestations can appear and the use of oral nonsteroidal anti-inflammatory medications, high-dose systemic steroids or other immunosuppressive drugs (e.g., cyclosporine) are often initiated and used for several months.7
Biguanides are the most effective drugs for this type of infection, including PHMB (polyhexamethylene biguanide 0.02-0.06%) and chlorhexidine 0.02%-0.2%. Our patient was started on PHMB, but had to be changed to chlorhexidine due to pain and intolerance.
Examples of diamidines include brolene (propamidine isethionate, 0.1%), desomedine (hexamindine diisethionate, 0.1%), corneal transplantation, photorefractive excimer, crosslinking and steroids.
Steroids remain controversial in treatment of AK, as there is no clear consensus about their use. They are often recommended in cases with a persistent infection with inflammation; however, they are controversial because they do suppress the patients’ immunological response. Studies have shown an association with topical steroid use and a diagnostic delay in AK manifestation, which was seen in our patient.5
Remember that your contact lens wearers will often present late because they are accustomed to having minor irritation due to the lenses. The most important factors associated with AK outcomes are disease severity at presentation and time to therapy initiation. A delay of three weeks is associated with worse prognosis; if you have any suspicion of AK, an attempt to get confirmation is necessary.8
This case ended up being complex, resulting in over 50 visits, with the patient seen by multiple specialists. She is still being seen today.
1. Page MA, Mathers WD. Acanthamoeba keratitis: a 12-year experience covering a wide spectrum of presentations, diagnoses and outcomes. J Ophthalmol. 2013;2013:670242. 2. Visvesvara GS, Moura H, Schuster FL. Pathogenic and opportunistic free-livin amoebae: Acanthamoeba spp., Balamuthia mandrillaris, Naegleria fowleri and Sappinia diploidea. FEMS Immunol Med Microbiol. 2007;50(1):1-26. 3. He YG, McCulley JP, Alizadeh H, et al. A pig model of Acanthamoeba keratitis: transmission via contaminated contact lenses. Invest Ophthalmol Vis Sci. 1992;33(1):126-33. 4. Patel A, Hammersmith K. Contact lens-related microbial keratitis: recent outbreaks. Curr Opin Ophthalmol. 2008;19(4):302-6. 5. Villani E, Baudouin C, Efron N, et al. In vivo confocal microscopy of the ocular surface: from bench to bedside. Curr Eye Res. 2014;39(3):213-31. 6. Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite. 2015;22:10. 7. Maycock NJ, Jayaswal R. Update on Acanthamoeba keratitis: diagnosis, treatment and outcomes. Cornea. 2016;35(5):713-20. 8. Dart JKG, Saw VPJ, Kilvington S. Acanthamoeba keratitis: diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148:487-99. |


