 |  |  |
In our profession, we have the opportunity to provide both an alternative to spectacle lens wear and a solution to compromised vision. As a result, we have seen the number of patients interested in contact lenses climb each year. Assuming a patient is a good candidate for contact lenses, we are able to provide a relatively straightforward fit thanks to the ever-expanding lens parameters available.
Although correcting ametropia is the main focus of most eye care providers and contact lens prescribers, it is important to think beyond vision correction for normal corneas and consider ways we can use contact lenses to improve vision and comfort for patients with corneal pathology.
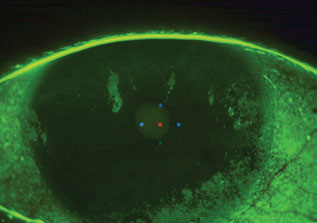 |
| Severe keratitis patients can benefit from daily disposables. Click image to enlarge. |
Contact Lenses by Condition
Of course, there are numerous potential categories worthy of discussion, but we’ll focus on a few of the most common.
Dry Eye. The treatment and management of dry eye disease has quickly become an important topic in eye care, not just for practitioners. Patients referred into our dry eye clinics are more informed now than ever about contact lens options for their dry eyes. While contact lenses do provide comfort for patients, they do not treat the disease process of dry eye.
In many severe cases, despite the best treatment protocol and patient compliance, it remains difficult to control corneal staining. Not only can this be incredibly uncomfortable for the patient, but it can also hamper their vision if the visual axis is involved. These patients’ corneas need protection from the desiccating stress causing corneal staining. This is where soft, daily disposables (used as a bandage contact lens) and scleral contact lenses come into play. Sclerals have several advantages over bandage contact lenses and tend to be our preferred choice when considering contact lenses for dry eye.
Scleral contact lenses protect a larger surface area of the eye, as the diameter can cover up to 24mm, as opposed to a standard soft lens, which typically only covers a maximum of 15mm. Most scleral lenses are made with gas permeable materials that can be coated to minimize deposits and improve wettability—unavailable in soft contact lenses. Patients who have tried both often state that scleral lenses feel more comfortable and less dry throughout the day. Scleral lenses, however, cost more than soft lenses, since each lens is individually designed for optimal fit, and require more dexterity for insertion, as these lenses are larger and can’t have bubbles upon insertion.
Though these lenses may help with patient symptoms, they generally do not treat the cause of the disease. For example, this modality does not allow the meibomian glands to regain function if compromised or actively decrease inflammatory dry eye. These problems should be addressed and treated prior to fitting contact lenses for dryness.
 |
| This patient is experiencing lagophthalmos. Click image to enlarge. |
Exposure Keratopathy. We also find it useful to fit contact lenses on patients with severe exposure keratopathy, such as that resulting from Bell’s palsy, which involves the seventh cranial nerve. As the duration of Bell’s palsy is generally short, with the patient typically fully recovering within three to six months, soft daily disposable lenses are usually the most reasonable choice.
Anterior Basement Membrane Dystrophy (ABMD). When working with this corneal disease, it is common for the surface of the cornea to become irregular and fail to tightly adhere to the underlying stromal tissue. This can cause surface irregularity, which disrupts clear vision, necessitating contact lenses to maximize vision.
There are several contact lens options worth considering to alleviate visual complaints secondary to ABMD. For mild cases, soft lenses with a higher modulus, such as those made from silicone hydrogel materials, help normalize corneal surface irregularities. For moderate to severe ABMD, gas permeable lenses tend to provide better optics, as they negate most, if not all, of the subtle irregularities associated with the post-lens tear film.
 |
| There are several lens options for patients with ABMD. Click image to enlarge. |
Corneal Erosions. ABMD can cause these erosions, which may result in debilitating pain. Extended-wear contact lenses are best in these situations, as they accommodate continual wear for several weeks while the corneal erosion re-epithelizes and re-adheres to the underlying stroma. The main goal is to minimize discomfort. It is common for recurrent erosions to occur, and, in these cases, amniotic membranes can promote healing and hemidesmosome formation, which allows the regenerating corneal epithelium to anchor and stabilize.1
When eye care providers think about contact lenses for compromised corneas, corneal ectasia, post-surgical cornea and corneal scar and opacity management are the first to come to mind. Our stories of patients who are finally able to see clearly after being fit with specialty contact lenses, and become emotional in our chairs, are what keep contact lens prescribers going. Our impact does not have to be life-changing; if we can improve a patient’s ocular discomfort or visual clarity, then we have succeeded in providing optimal service and care.
Dr. Fischer completed his residency in cornea, specialty contact lenses and dry eye at Specialty Eye in Seattle in 2019. He practices at Professional Eyecare Associates in Huntingburg and Jasper, IN, and leads the Dry Eye and Specialty Contact Lens Clinic within the practice.
1. Resch MD, Schlötzer-Schrehardt U, Hofmann-Rummelt C, et al. Adhesion structures of amniotic membranes integrated into human corneas. Invest Ophthalmol Vis Sci. 2006;47(5):1853-61. |


