 |
With the start of the new year comes new year’s resolutions. Whether you make them in anticipation of breaking a bad habit or just for a general resetting of priorities, resolutions give us a chance to focus on what we wish to do better in the year ahead. For 2021, consider going back to the basics. What must we do well to fit GP lenses in the most efficient and accurate manner possible? How can we reduce the trials and tribulations of fitting and increase the happiness these lenses bring to our patients and practices? Here are some possible resolutions you can make (or break) this year.
The present visit opened up a much-needed dialogue, and we were able to mutually agree that changes to her routine and lenses were necessary. In the decade since her last visit, advancements in contact lens designs and care have allowed us to better meet her needs.
 |
Put your diagnostic GP lens in a non-neutralizing case filled with ophthalmic-grade hydrogen peroxide solution for disinfection. Click image to enlarge. |
Verify Diagnostic Lenses
Prior to starting a new diagnostic fit, it’s a good idea to verify the parameters of the diagnostic lens you will apply. This will not only ensure the lens is not chipped, cracked or damaged but also save you grief later. Signs your chosen lens might be incorrect include making a diagnostic lens change where the fit doesn’t respond as anticipated or if your expected over-refraction doesn’t pan out. Key parameters to verify include lens power (easily accomplished on a standard lensometer) and base curve (using a radiuscope). Less important is the lens diameter, though you could easily verify this in seconds using a 7x contact lens magnifier or a diameter gauge.
While you’re at it, consider verifying your entire library of diagnostic lenses. Consider assigning a staff member to handle this task on a regular basis. This person will become an expert at lens verification, which is useful for other tasks, such as checking in ordered lenses or confirming a patient’s habitual lenses.
If you’re in the market to purchase a new diagnostic lens fitting set, ask your lab to manufacture a custom set for your practice that contains lenses in different material colors to hasten the verification process. Have all the brown lenses be of one design or all the green lenses take up one row in the diagnostic set. Make even-numbered base curves in clear material and odds are blue. Better yet, request that your diagnostic lenses come laser-marked with their parameters or an alternate code that you specify.
Focus on Disinfection
I highly recommend disinfecting each of your diagnostic lens sets according to the latest standards and recommendations. More details on diagnostic lens disinfection can be found in my September/October 2020 column. A convenient flow chart is also available on the American Academy of Optometry website’s “My COVID Hub” section. In short, after a GP lens is used on-eye, clean it, place it in a non-neutralizing case with 3% ophthalmic hydrogen peroxide solution, let it soak for three or more hours, rinse it with multipurpose solution, pat it dry, and then store it dry. Note that diagnostic hybrid and soft lenses follow an alternate protocol not outlined here and should undergo re-disinfection every 28 days.
Lenses that undergo disinfection should also be logged so that they can be tracked in case a subsequent infection is diagnosed that was present during fitting. For example, diagnostic lenses should be discarded (and not used again) in patients with hepatitis, HIV, prion disease, herpes ocular infection, adenovirus or Acanthamoeba keratitis.1,2
The information in the record can be used to contact patients later fit with the same diagnostic lens, to advise them of potential risk. If you do not currently have a standardized process for lens disinfection and logging in your office, now is the time to start. Assign a staff person to handle these tasks on a daily, weekly, or monthly basis as well.
Offer to Presbyopes
We know those with irregular corneas, high ametropia or moderate-to-high amounts of astigmatism are excellent candidates for GP lenses. Presbyopes who currently wear GP lenses are no-brainer candidates, too—but don’t forget about neophyte wearers. You owe it to patients to discuss all potential options, and sometimes I’m surprised at the quick adaptation once they achieve freedom from reading glasses.
Depending on the degree of presbyopia, you may consider different designs. For emerging presbyopes, a simultaneous multifocal design can provide full correction in both eyes (as opposed to monovision, which does not). For mid-to-late presbyopes, both simultaneous and translating designs can provide sufficient near add. Within the multifocal fitting process, if you need additional plus, there are also fitting options to enhance distance or near (similar to modified monovision), or you can recommend top-up spectacles to provide additional plus. It’s good practice to give the patient permission to wear spectacles over the lenses as needed for demanding near tasks.
Collect Thorough Data
Remember the old saying, “garbage in, garbage out”? That’s the case with empirical fits of GP lenses. If you don’t gather good data on the front end, you won’t have a successful empirical fit (or you’ll leave your lab consultants confused on how to help you).
With any new fit, gather the appropriate data at the initial visit, including (at a bare minimum): keratometry readings, refraction, horizontal visible iris diameter and lid position. If you’re fitting a multifocal, also gather the patient’s near add power, pupil size and dominant eye and critically assess lid position and tone. A topography map can be useful, but is not required, and may help with habitual wearers than new wearers, where you can rule out conditions such as corneal warpage or molding. Of course, if you suspect ectasia, a tomography map is the key a problem-related diagnostic test. Assessment of tear quality and quantity, which may be reduced in the presbyopic age group, also warrants attention and associated treatment in the pre-fit phase.
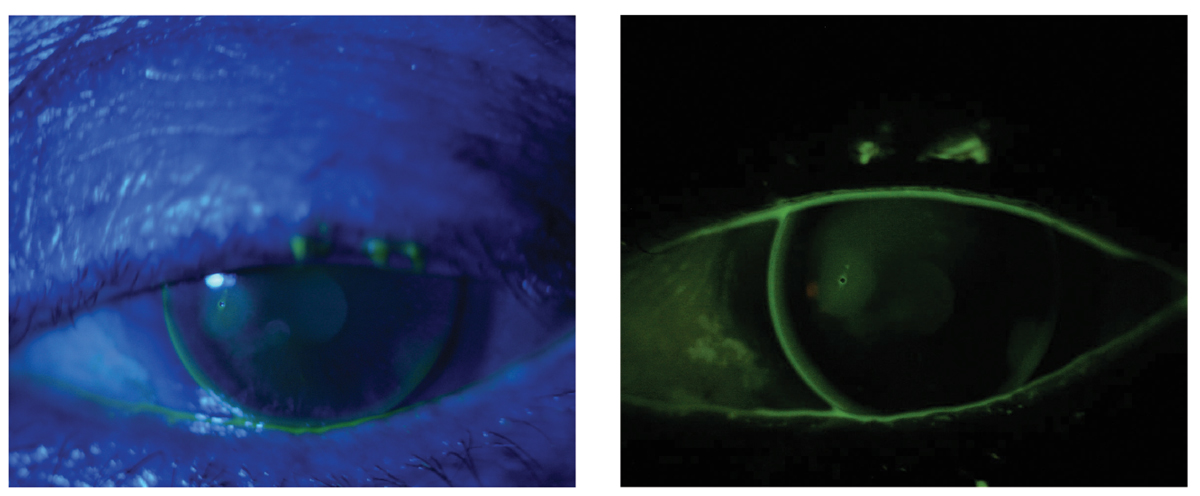 |
The same lens is viewed with blue light (left) and then with a wratten filter (right). The filter highlights a small area of pooling with dimple veiling over a corneal scar in the temporal cornea. Click image to enlarge. |
Assess Lens Completely In-Office
When assessing lenses on dispense or follow-up, perform a complete evaluation. Referring to detailed notes can be useful later on, whether you are trying to verify a new finding or consulting with the laboratory on lens changes. When fitting GP lenses, record all aspects of the fit, including blinking (full or partial), lens position (lid attached, interpalpebral), centration (or direction of decentration), movement (in millimeters) and lens condition (note any surface scratches, debris, deposits or lens markings).
Instill sodium fluorescein and determine the fitting relationship using blue light. A Wratten filter can help quickly identify any subtle areas of touch or pooling.
Ensure Appropriate Care
For new GP lens wearers, it is rather obvious that follow-up visits are necessary to ensure appropriate adaptation to lens wear. After-care visits also give us the opportunity to review proper practices for lens wear and care, including proper use of solutions. Through appropriate questioning, we can confirm the patient is happy with the outcome and answer any outstanding questions. Even in fits where the patient is a habitual GP lens wearer, if I make significant changes in base curve or edge design, I prefer a follow-up visit to confirm the eye is adapting well and the fit remains as expected at the end of the day.
Whether you love or hate resolutions, the new year gives you a chance to make changes in your contact lens practice. I wish you a year of happy fittings!
1. Sindt CW et al. Technical Report: Guidelines for Handling of Multipatient Contact Lenses in the Clinical Setting. Optom Vis Sci. 2020. 2. International Organization for Standardization. (2018). Ophthalmic optics—contact lenses—Hygienic management of multipatient use trial contact lenses. www.iso.org/standard/67859.html. March 2018. Accessed January 13, 2021. |


