|
I have had a few cases recently that have really made me wonder whether a return to fitting more corneal lenses may just improve my doctoring life. For the time being, let’s look at patients who just didn’t get along with their soft contact lenses. Some of these patients are currently taking a break from lenses as a whole, and others we have managed to refit—either into a different material or modality of soft contact lenses, or, into my personal hero, corneal lenses! In all cases, corneal gas-permeable (GP) lenses are an incredible option to consider, for reasons we will explore.
Case #1: Giant Papillary Conjunctivitis
KH, a 17-year-old African-American young man, developed symptoms of gradually progressive eye irritation over the last 10 months. He reported wear of weekly soft contact lenses for the last five years. He was unsure of the brand or power. He reported using generic multipurpose solution. The average wear time was 12 hours per day, seven days per week, with replacement approximately every two weeks. He reported the entering pair was “about two weeks old” and bothering him. He had backup spectacles but did not bring them to the visit. Medical history was positive for asthma, for which he was not taking any medication. He reported an allergy to amoxicillin.
Slit lamp examination revealed giant papillae in both eyes, graded as 2 to 3+ on the lower lid and 3 to 4+ on the upper lid. Of note, there was apical scarring of the 4+ papillae on the left upper lid (Figure 1). The lid was easily everted. The manifest refraction was OD -3.75 -0.50x125 and OS -4.25 -0.50x060. The patient was diagnosed with both giant papillary conjunctivitis OU and floppy eyelid syndrome OU. He was started on a topical steroid and an over-the-counter antihistamine/mast-cell stabilizer. He was also started on nighttime artificial tears ointment with lid taping. Once quiet, this patient would have been a good candidate for refit into a corneal GP lens design.
 |
|
Fig. 1. Upper lid eversion of patient in case 1, showing giant papillae with scarred apices. Click image to enlarge. |
Case #2: Limbal Stem Cell Deficiency
MT, a 14-year-old Hispanic girl with degenerative myopia, developed symptoms of gradually progressive discomfort with soft contact lens wear over the last year. She admitted to overwear of her habitual daily disposable multifocal lenses for three or more days at a time. A review of the purchase history indicated that over the past 4.5 years of reported daily wear, the family had purchased a total of 17 months’ worth of lenses. She denied being seen at any outside provider or purchasing lenses elsewhere or online during that time.
 |
|
Fig. 2. Superior corneal appearance of patient in case 2, showing sawtooth staining pattern characteristic of limbal stem cell deficiency. Click image to enlarge. |
The patient denied ever sleeping in the lenses. The average wear time was 12 hours per day, seven days per week. She reported the entering pair was new today, from an extra box they had at home. She had backup spectacles but did not like wearing them as she was bullied in class due to their thickness. The patient had no medical conditions and was not taking any medications. She reported no known allergies.
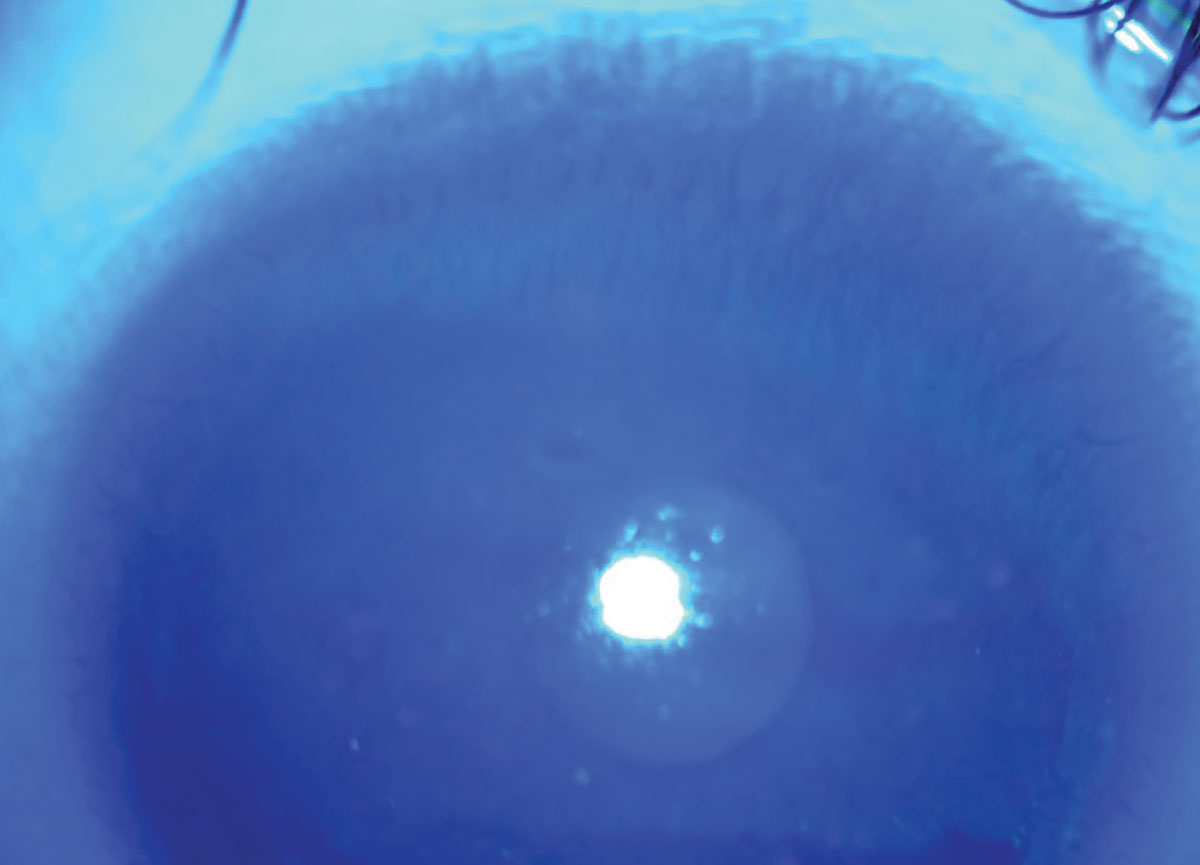
Slit lamp examination revealed a tight-fitting soft contact lens in each eye with no movement in primary or upgaze. A soft lens push-up test was difficult in each eye. The cornea had limbal neovascularization in all quadrants. Sodium fluorescein staining after lens removal revealed 1+ arcuate conjunctival staining indicating a tight-fitting lens. There were also nasal and temporal punctate epithelial erosions in each eye and a sawtooth staining pattern was identified superiorly at the limbus OU (Figure 2).
The manifest refraction was OD -15.75 -3.00x180 and OS -17.00 -0.75x175. A Pentacam scan confirmed corneal warpage was present from the tight-fitting lens in each eye (though it is important to note this type of corneal warpage can masquerade as keratoconus/corneal ectasia). The patient was diagnosed with limbal stem cell deficiency OU due to contact lens overwear. She was started on topical steroids and advised to discontinue wear of her habitual lenses. Once quiet, this patient would have also a good candidate for refit into a corneal GP or scleral lens design to prevent further exacerbation of the limbal stem cells.
 |
|
Fig. 3. Corneal neovascularization seen in the patient in case 3. Click image to enlarge. |
Case #3: Contact Lens Overwear
FS, a 53-year-old African-American man with degenerative myopia, developed symptoms of blurry vision and discomfort with a two-year-old pair of monthly replacement, spherical, soft contact lenses. The patient reported he became homeless and was unable to go back to where his lens supply was kept. He also had trouble finding a place to consistently remove and clean his lenses. He instilled artificial tears for contact lenses as needed, which provided some relief to the blur and discomfort. The patient admitted to sleeping in his lenses six or more nights per week. He had a history of both soft toric and scleral lens wear. He denied having any backup spectacles. The patient has a history of heart failure and COPD and is on furosemide 40mg per day. He reported no known allergies.
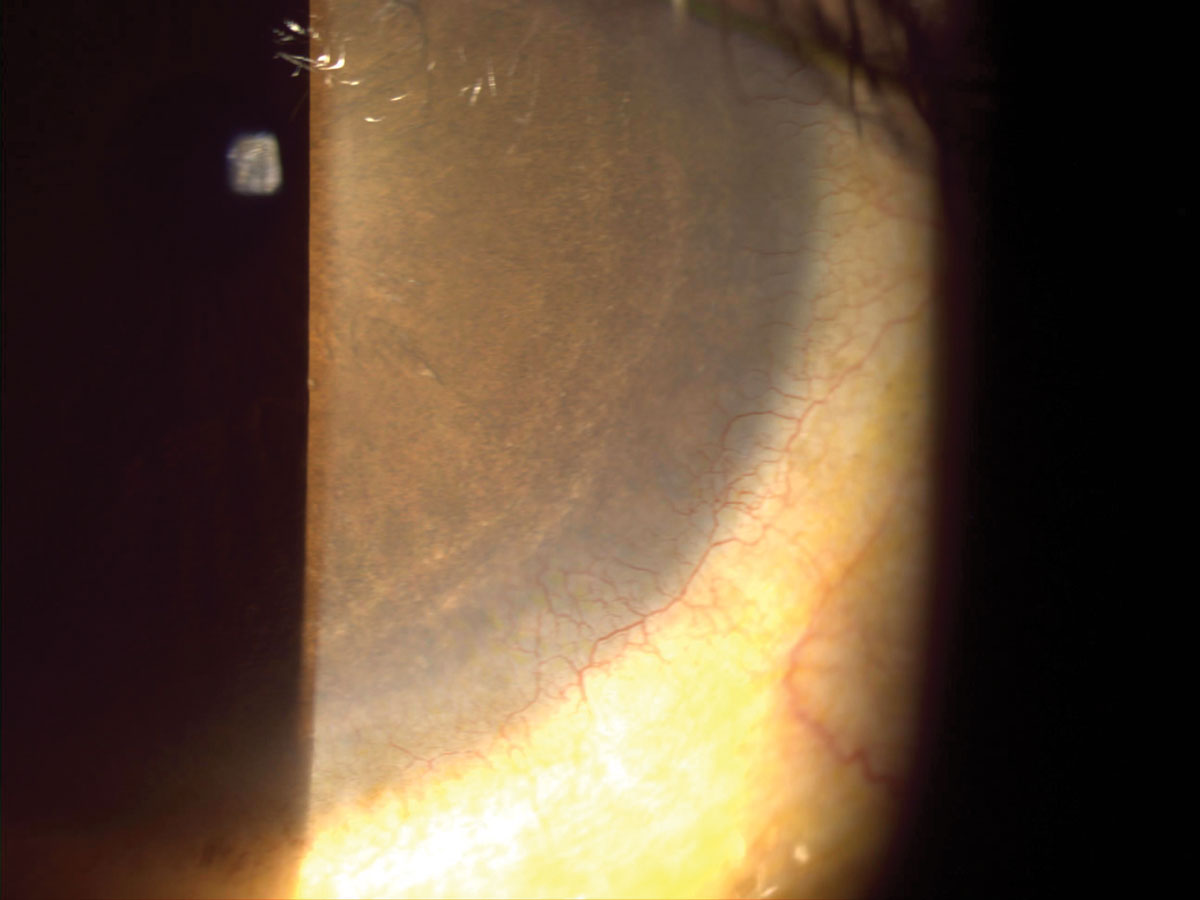
Slit lamp examination revealed 1+ MGD on the upper and lower lids, 1+ diffuse bulbar conjunctival injection, 2+ palpebral conjunctival papillae and injection, and neovascularization in all quadrants OU (Figure 3). There was a faint anterior stromal scar in the right eye, and 2+ diffuse punctate epithelial erosions in each eye after lens removal.
The manifest refraction was OD -12.00 -2.50x180 and OS -13.00 -3.00x065. He was started on an antibiotic-steroid topical drop, along with preservative-free artificial tears. He was advised to stay out of his contact lenses as much as possible, and a prescription for backup glasses was dispensed.
Once quiet, this patient may have been a good candidate for refit into a corneal GP lens for extended wear in a hyper-Dk material. This would allow him to not only correct all of his refractive error but also allow for flexible wear while preventing worsening of the neovascularization.
Each of these cases presents a soft contact lens fit causing problems for the patient. While short-term lens discontinuation might be wise in these cases, these patients can successfully return to contact lens wear. Often, a well-fitting corneal lens is the answer to help the patient do so in a safe manner for their ocular health.