 |
When discussing solutions with patients, how do you ensure proper compliance with your recommendations? We always strive to provide thorough education at the initial visit. We may recommend purchase of specific items and through specific channels (e.g., online, in-office purchase). Regardless of how carefully worded our instructions, or how thoughtful our recommendations, patients can still be led astray by incorrect recall or faulty logic.
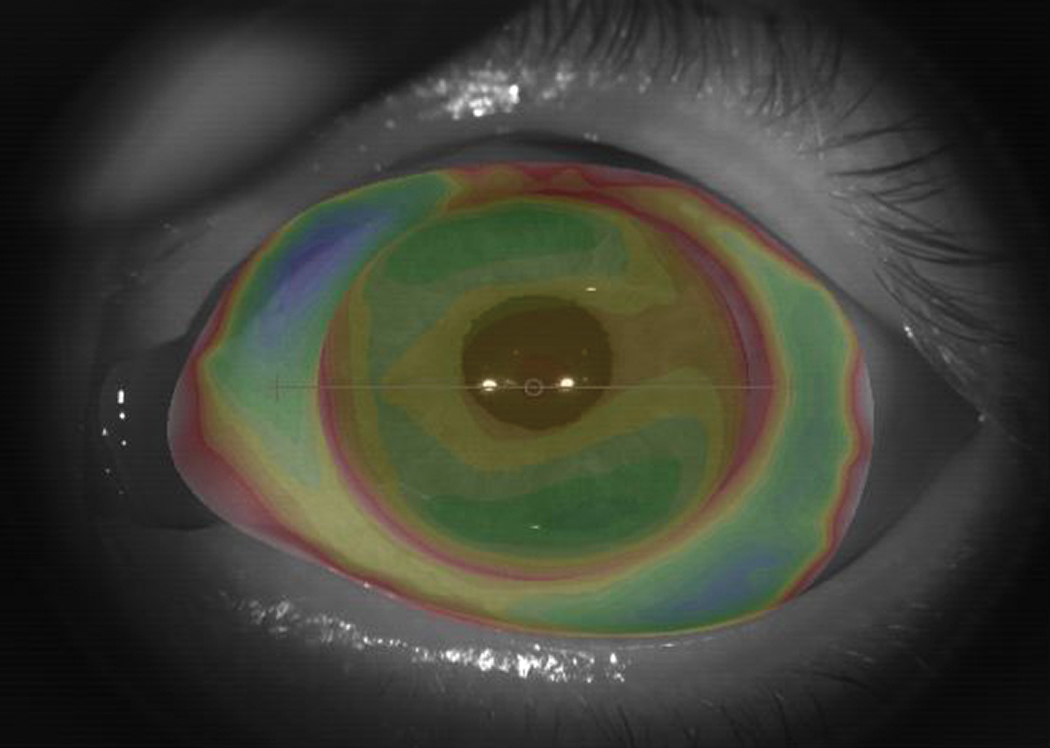 |
Fig 1. This profilometry image helped design our patient’s scleral lens. Click image to enlarge. |
Early Troubles
Recently, I had the privilege of fitting a family friend with keratoconus in scleral lenses for the first time. After failing in corneal lenses seven years ago, this 34-year-old was hesitant. I reassured him that we would work together to achieve success, and I felt his odds would be improved with scleral lenses.
His spectacle refraction was -4.25 -1.00 x 080 OD with a VA of 20/70 and -2.50 -1.75 x 150 OS with a VA of 20/30. Minimum pachymetry values were 430µm OD and OS 472µm OS. We fit Valley Contax Custom Stable Elite 15.8mm scleral lenses, designed using profilometry scans from the Eaglet Eye Surface Profiler (Figure 1). His deep-set eyes made obtaining sufficient maps in the vertical meridian more challenging, but we were able to obtain an adequate fit after exchange.
His newfound distance vision with scleral lenses was 20/20 OD and 20/25 OS. When he took the lenses home, I let him know he could text me at any time with questions. I was amazed at what he asked when given all-hours access. This patient contacted me to confirm which eye drops were appropriate for use and when to discard preservative-free saline. He was also not correctly rinsing his lenses with hydrogen peroxide solution before soaking, nor was he using that solution daily. His lenses were coated in a commercially available surface coating specially designed to improve lubricity, and his leaving them dry in the case every other night was problematic. Lack of adherence to appropriate procedures resulted in post-lens tear reservoir debris and front surface non-wetting (Figure 2).
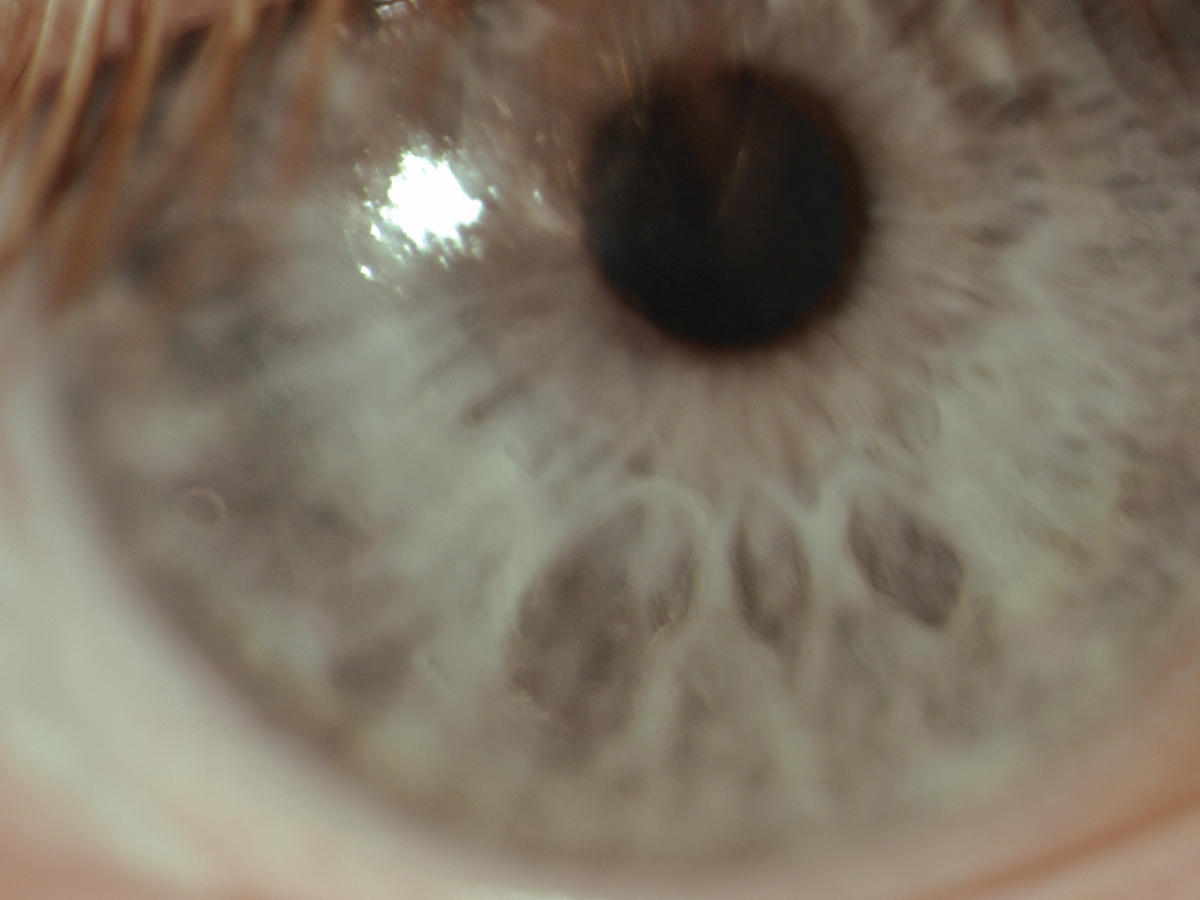 |
Fig. 2. This front surface non-wetting of the scleral lens was caused by lack of adherence to solutions regimen. Click image to enlarge. |
Thorough Education
This scenario left me feeling a bit embarrassed at how I had failed to properly emphasize critical lens care items. With patients like this in mind, here are some strategies to overcome common pitfalls when confronting patient compliance with contact lens solutions.
Ensure your technicians and staff are highly trained. Consider training all staff to instruct patients in the same way you would. This means ensuring staff is familiar with the proper protocols for each solution you prescribe. “Is there a rinse step? How long is the rubbing step? What should the patient do if they drop a lens in the sink or on the floor? When should solutions be discarded? What if the tip of the bottle is contaminated? How do I clean my case? Can I use water to rinse my lenses?” These are critical questions staff should anticipate and prepare for, whether they pertain to GP, soft or other specialty lenses.
Place emphasis on the intricacies of each particular solution during training. Solutions carry varied recommendations for the required rub and rinse steps. Specifics for each brand can be found on the package insert. For new wearers, this information is critical to enforce proper protocols. For previous wearers, this information can dispel old myths or correct bad habits. For all wearers, these steps reduce the bacterial bioburden on the lens and reduce the incidence of complications.
Sometimes the latest research has recommendations that differ from the package insert. For example, some solution package inserts still contain the now ill-advised recommendation to rinse GP lenses with tap water. Another one is a recent study that suggests rubbing is essential to remove stubborn oily deposits from orthokeratology lenses even if using a hydrogen peroxide system.1
Incorporate video education. Using videos to deliver key points in the contact lens care regimen can help ensure consistency and incorporate visuals with your message. You can use videos that are readily available, such as those from solution manufacturers, contact lens manufacturers or educational societies. For a low-cost custom option, create your own videos and have your staff members star in them. Outline scripts where you include the key points you wish to address. Don’t forget to reinforce the importance of thorough handwashing before and after lens handling.
Give written instructions. Whether provided by a manufacturer or drafted specifically for your practice, handouts supply patients with a tangible reminder of the knowledge they’ve gained during training. These instructions, when vetted by the practitioner, are much better for patient education than anything your patient may find online. You probably don’t want patients navigating random YouTube videos or online forums in a panic! Ensure the signs and symptoms of potential infection are highlighted on any handouts and include your office emergency contact for any questions that may arise.
Prescribe solutions to patients. Consider your patient’s lenses and make a single recommendation for which solution you believe will work best. Whether it’s a two-bottle (cleaner/conditioner), a multipurpose or a hydrogen peroxide based system, avoid giving multiple options. The last thing you want to do is give your patient “choice overload.” You are the expert in what solutions work best with which lens materials and patient scenarios. While you may not have a prescription pad handy in the era of electronic health records, you can still prescribe a solution that will best meet the patient’s needs. Follow-up on these recommendations at each aftercare visit so you can troubleshoot issues that arise, such as preservative sensitivity or improper procedures.
Review proper procedures at each aftercare visit. If you are not personally doing the case history at each contact lens aftercare visit, get in the habit of asking patients which lens solutions are being used. Confirming these items, even mid-exam, can reveal crucial discrepancies.
I sometimes find the same solution listed in the chart for the last several visits, but, suddenly, the patient changes their routine. “I got this other type of saline because I thought it was the same.” “I borrowed this new kind of solution from my sister.” “This brand was on sale last week, so I bought a twin-pack.” “I found an old, travel-sized bottle of lens solution under my sink.” You name it, we’ve heard it—so we still need to take the time to ask.
Have the patient show and tell. One additional strategy to ensure proper compliance is to have patients show you what they are doing. Patients may hesitate (because it feels like a test) but encourage them to keep going. If your patient is shy, at least have them talk you through the steps they take in their care regimen. Gently point out any places they could improve and correct the procedures where indicated.
Ask if there are any questions. After patient education is complete and the patient is ready to leap out of your chair, stop and ask if there are any remaining questions. The strategy here is to use the phrase, “What questions do you have for me?” rather than, “Do you have any questions?” It’s a classic positive psychology tactic. You are giving the patient permission to ask questions. When you say, “Do you have any questions?” the tendency is to say “Nope!” and end the conversation. Avoid that abrupt ending and welcome the patient’s inquiries by extending them permission to continue.
Solutions compliance will continue to be a challenge in our practices for all types of patients, new and established. Incorporating strategies to improve compliance now can help drive comfortable lens wear for your patients for years to come.
1. Cho P, Poon HY, Chen CC, Yuon LT. To rub or not to rub?–effec gid contact lens cleaning. Ophthalmic Physiol Opt. 2020;40(1):17-23. |


